Health Information
Diabetes

Preventing Type 2 Diabetes

- Move more. Walk, dance, or ride a bike with your friends or family.
- It doesn't matter what activity you do, as long as you enjoy it.
- Choose healthy foods. Eat fiber-rich fruits and vegetables.
- Maintain a healthy weight. With healthy eating and more physical activity, you can drop pounds and keep them off.
- Set reasonable goals. Start with small changes, like being active for 15 minutes a day this week.
- Add 5 minutes per day, each week until you're up to at least 30 minutes, 5 days a week.
- Record your progress. Keep a diary of what you eat and drink and the number of minutes you exercise.
- It's a great way to stay focused and reach your goals.
- Keep at it. Making even small changes is hard in the beginning.
- If you get off track, start again
Depression
- Sadness
- Loss of interest or pleasure in activities you used to enjoy
- Change in weight
- Difficulty sleeping or oversleeping
- Energy loss
- Feelings of worthlessness
- Thoughts of death or suicide
Back Pain
Is your back hurting? You’re in good company. In any 3-month period, about 1 in 4 adults in the U.S. has at least one day of back pain, mostly in the lower back.
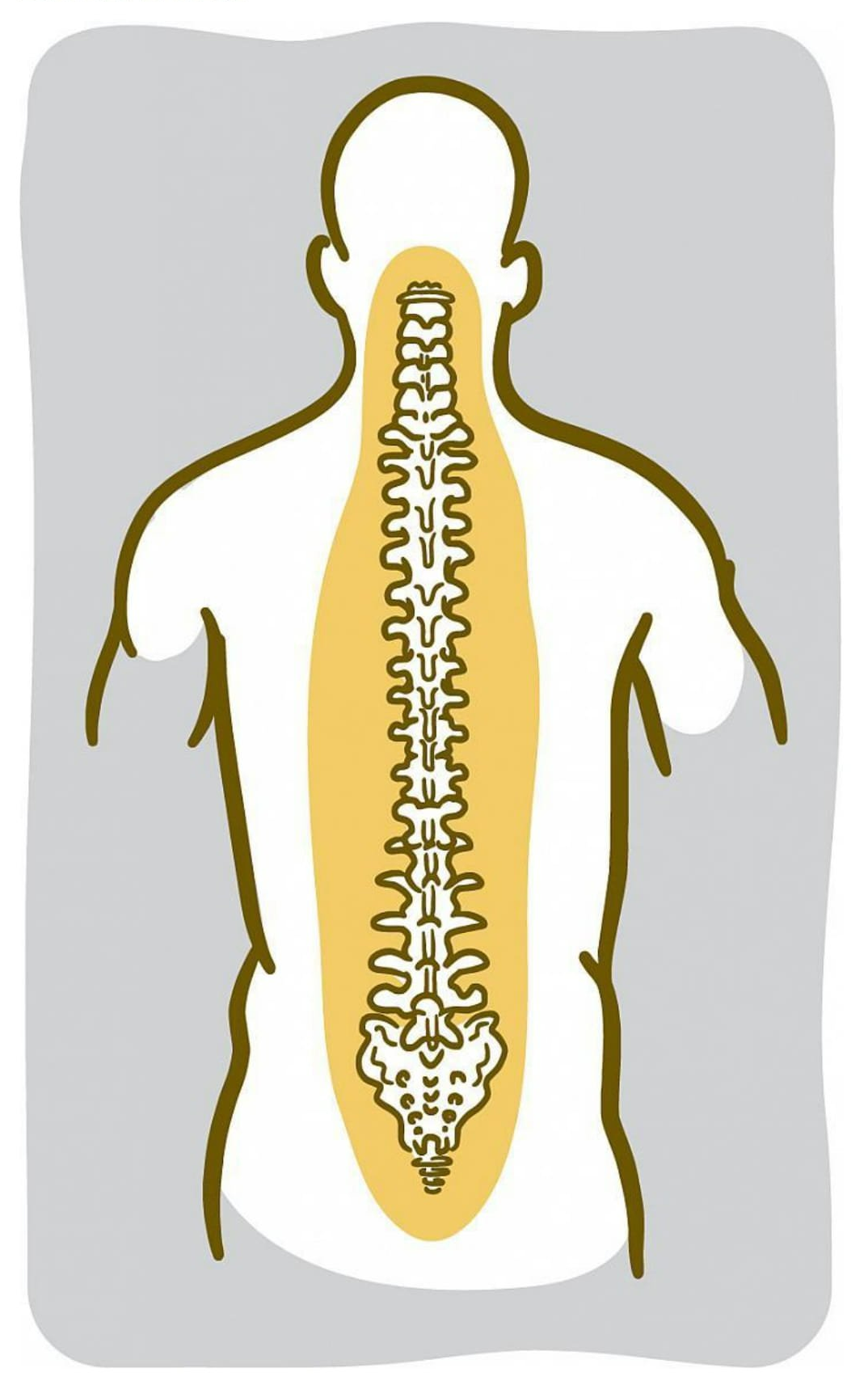
The back is a complicated structure. Its center is the spine, which is made up of 33 bones called vertebrae, stacked in a column. The nerves of the spinal cord run in a tunnel through the middle of those bones. Spongy discs between the vertebrae act as cushions. Ligaments and tendons hold everything together.
A lot of things can go wrong with your back. A strained muscle or a problem with a disc or a bone can cause pain. Back pain might also arise from a fracture or tumor. Much of the time, though, it’s impossible to tell what’s making your back hurt.
“We rarely find out exactly what it is,” says Dr. Gunnar Andersson, an orthopedic surgeon at Rush University Medical Center in Chicago. “As long as it stays as back pain, we are typically not that concerned.”
Your back naturally changes as you get older. Discs degenerate and arthritis may develop in the small joints of the back. Those changes may show up on an MRI or other types of imaging scans. But such changes to the back are also seen in a lot of people who don’t have back pain. So it’s hard to know if the changes are actually what’s causing the pain.
People with obesity are more likely to have low back pain, as are people who smoke. Back pain is also more common in people who don’t exercise much, or in people who are mostly inactive but have occasional bursts of exercise.
The good news is most back pain goes away by itself. For a new pain in the back, Andersson says he usually advises taking over-the-counter medications for the pain and staying away from activity that is hard on the back—lifting, carrying, bending, and twisting. “Then, wait for the problem to disappear, which it will in the great majority of people over a few weeks,” he says.
But for some people, the pain continues. If your back hurts most of the time for more than 3 months, you have chronic back pain.
What doctors do about chronic pain depends on the source of the pain. Some chronic back pain requires prolonged medical attention. If the pain comes from a fracture or tumor, those problems can be treated. Surgery can help if the pain is caused by a ruptured (herniated) disc or certain other conditions like spinal stenosis (narrowing of the spinal column, which can put pressure on the nerves) or degenerative spondylolisthesis (when one vertebra slips over another). But surgery isn’t the right choice for everyone.
There are many treatment options for back pain, so be sure to talk to your health care provider about which approach is right for you. For most people, even chronic pain eventually clears up without surgery. The most important thing, Andersson says, is not to let the pain take over. Research has shown that patients who stay active are better off. Just be sure to avoid activities that might strain the back. “It’s important not to succumb to the pain and become afraid of moving,” Andersson says. "It doesn’t seem to make much difference what you do, as long as you stay active.”
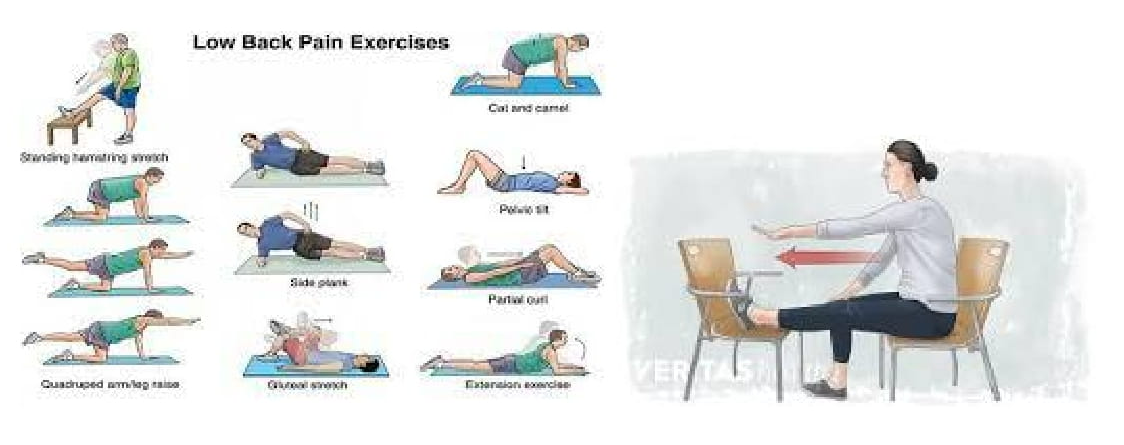
Strengthen your core muscles daily.
- Invest in an ergonomic office chair.
- Safeguard your back while lifting.
- Dissipate stressors during everyday activities.
- Rest your back after prolonged bending.
- Protect your discs immediately after waking.
- Stretch your hamstrings.
Colonoscopy
- To screen for colon polyps (growths of tissue in the colon) or colon cancer
- Rectal bleeding
- A change in bowel habits, like persistent diarrhea
- Iron deficiency anemia (a decrease in blood count due to loss of iron)
- A family history of colon cancer
- A personal history of colon polyps or colon cancer
- Chronic, unexplained abdominal or rectal pain
- An abnormal x-ray exam, like a barium enema or CT scan
- Water
- Clear broth (beef, chicken, or vegetable)
- Coffee or tea (without milk)
- Ices
- Gelatin such as Jell-o (avoid red gelatin)


- white rice, pasta, and bread
- mashed potatoes (no skins)
- canned fruits and veggies
- clear fruit juices (apple is best)
- Jell-o (but avoid red, blue, or purple coloring)
- clear soft drinks (like Sierra Mist or 7-up, many clinics even allow root beer!)
- coffee and tea (no milk or creamer)
- broth

- Keep the fluid cold
- Drink through a straw placed at the back of the mouth
- Suck on tart hard candies or lemon to mute the taste

Heart Diseases
Heart Attack or Stroke?
What To Do When Every Moment Counts
How would you react to a medical emergency? When it comes to life-threatening conditions like heart attack or stroke, every minute counts. Get to know the signs and symptoms of these health threats. If you think you or someone else might be having a heart attack or stroke, get medical help right away. Acting fast could save your life or someone else’s.
Heart disease and stroke are 2 of the top killers among both women and men in the U.S. Nationwide, someone dies from a heart attack about every 90 seconds, and stroke kills someone about every 4 minutes, according to the U.S. Centers for Disease Control and Prevention. Quick medical help could prevent many of these deaths. Fast action can also limit permanent damage to the body.
Heart attack and stroke are caused by interruptions to the normal flow of blood to the heart or brain—2 organs that are essential to life. Without access to oxygen-rich blood and nutrients, heart or brain cells begin to malfunction and die. This cell death can set off a series of harmful effects throughout the body. The changes ultimately lead to the familiar symptoms of a heart or brain emergency.

You might know the most common symptoms of heart attack: sustained, crushing chest pain and difficulty breathing. A heart attack might also cause cold sweats, a racing heart, pain down the left arm, jaw stiffness, or shoulder pain.
Many don’t know that women often have different heart attack symptoms than men. For instance, instead of having chest pain during a heart attack, women may feel extremely exhausted and fatigued or have indigestion and nausea.
“Many women have a vague sense of gloom and doom, a sense of ‘I just don’t feel quite right and don’t know why,’ ” says Dr. Patrice Desvigne-Nickens, an NIH expert in heart health.
The symptoms of stroke include sudden difficulty seeing, speaking, or walking, and feelings of weakness, numbness, dizziness, and confusion. “Some people get a severe headache that’s immediate and strong, different from any kind you’ve ever had,” says Dr. Salina Waddy, an NIH stroke expert.
At the first sign of any of these symptoms, fast action by you, someone you know, or a passerby can make a huge difference. NIH-funded research has helped ensure that more people survive heart attacks and strokes every year. We now have medicines, procedures, and devices that can help limit heart and brain damage following an attack, as long as medical help arrives quickly.
If the heart is starved for blood for too long—generally more than 20 minutes—heart muscle can be irreversibly damaged, Desvigne-Nickens says. “You need to be in the hospital because there’s a risk of cardiac arrest [your heart stopping],” which could be deadly. At the hospital, doctors can administer clot-busting drugs and other emergency procedures.
With stroke, Waddy says, “The longer you wait, the more brain cells are dying,” and the greater the chance for permanent damage or disability.
Emergency treatment for stroke depends on the kind of stroke. The most common type, ischemic stroke, is caused by a clot that clogs a blood vessel in the brain. The clot-dissolving drug tPA works best when given soon after symptoms begin. NIH research shows that patients who received tPA within 3 hours of stroke onset were more likely to recover fully.
Other strokes are caused by a hemorrhage—when a blood vessel breaks and bleeds into the brain. “The patient can have a larger hemorrhage within the first 3 hours,” Waddy says. A hospital medical team can help contain the bleeding, so every moment counts.
Even if you’re unsure, don’t feel embarrassed or hesitate to call 9-1-1 if you suspect a heart attack or stroke. “You should not go get your car keys. Your spouse shouldn’t be driving you to the hospital,” advises Desvigne-Nickens. “The emergency crew is trained to treat these symptoms, and it could mean the difference between life and death.”
Heart attack or stroke can happen to anyone, but your risk increases with age. A family or personal history of heart attack or stroke also raises your risk. But some risk factors for heart attack and stroke are within your control. Treating them can dramatically reduce your risk.
“If you have high blood pressure, high cholesterol, or diabetes, work with your doctor to get these conditions under control,” Waddy says. “Know your numbers [blood pressure, blood sugar, and cholesterol] and what they mean.”
You can also prepare for a medical emergency, to some degree. A hospital may not have access to your medical records when you arrive. Keep important health information handy, such as the medicines you’re taking, allergies, and emergency contacts. It would be important for the medical team to know, for example, if you’ve been taking anticoagulants to help prevent blood clots; these blood thinners put you at increased risk of bleeding. You might consider carrying an NIH wallet card that lists heart attack symptoms and has room for your personal medical information.
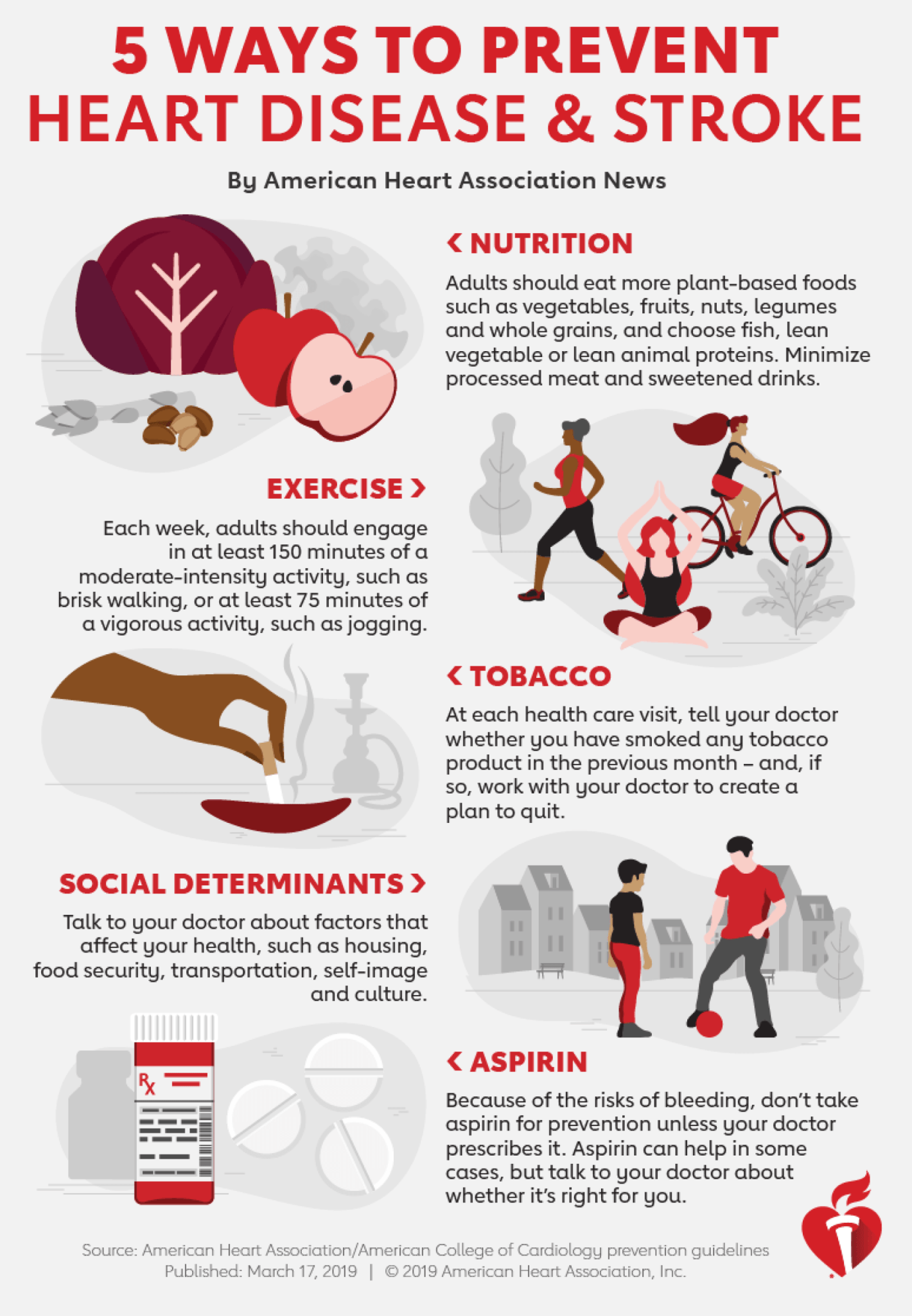
NIH researchers are studying new drugs and procedures to help the heart and brain repair themselves and improve organ function. “But there is absolutely nothing that will save both your time and health as well as prevention,” says Dr. Jeremy Brown, director of NIH’s Office of Emergency Care Research. Studies show that making healthy lifestyle choices can help prevent these medical emergencies from happening in the first place. Eat a healthy diet rich in protein, whole grains, and fruits and vegetables, and low in saturated fat. Get regular physical activity and don’t smoke.
“I think one of the most important things we can do is to take a basic CPR and first aid course,” recommends Brown. “We know the majority of cardiac arrests happen outside of hospitals and of that many, many can be saved if we get people with basic training on the scene quickly. An ambulance can never get there as quickly as a citizen passing by.” Whether or not you’re trained to offer help, if you see someone having symptoms of a heart attack or stroke, call for help immediately. “If you’re even thinking about calling 9-1-1, you should call,” Desvigne-Nickens says. “Yes other conditions can mimic the signs and symptoms of a heart attack or stroke, but let the emergency physician figure that out in the emergency room.
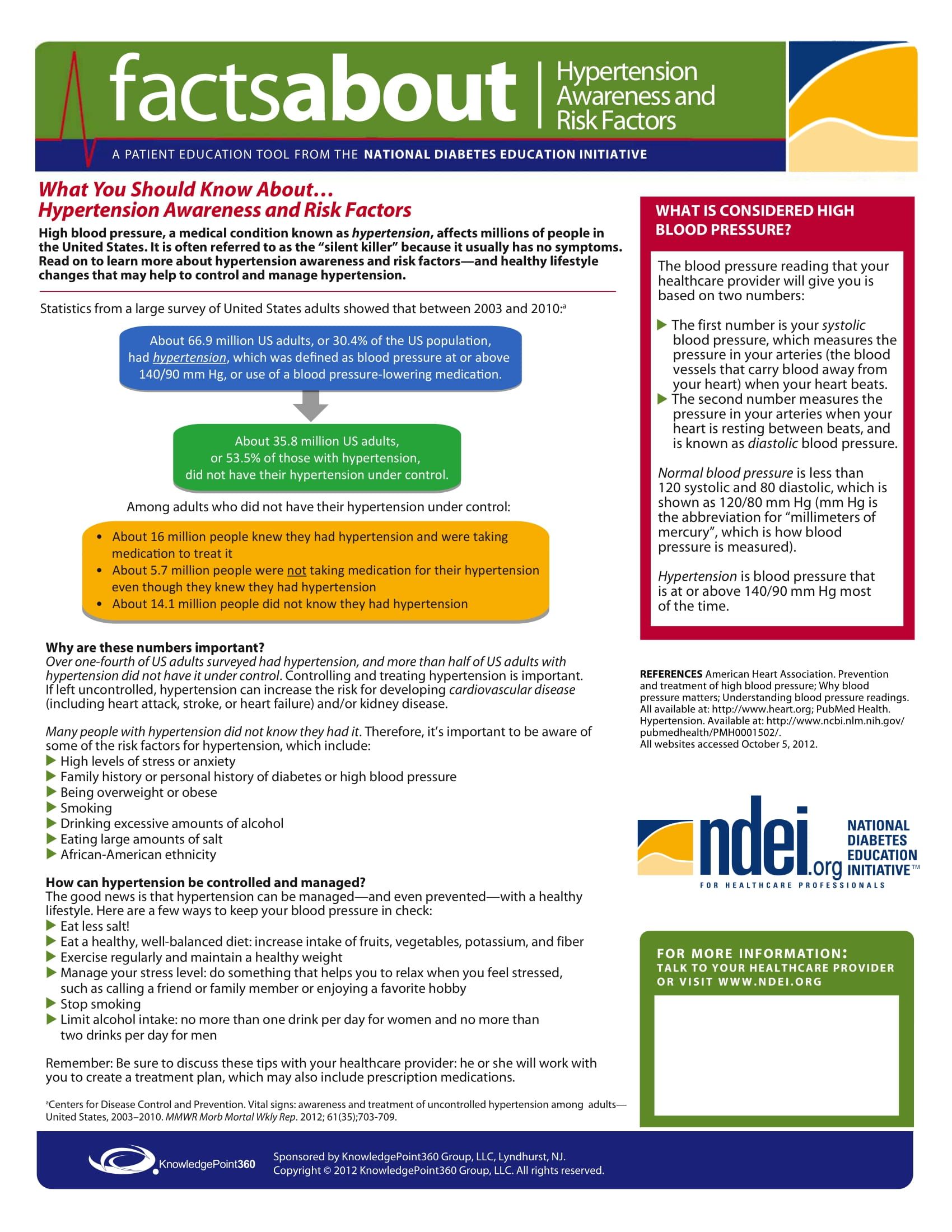
High Blood Pressure
- Reducing your sodium (salt) intake: If you have high blood pressure, diabetes, or chronic kidney disease, or you’re middle-aged or older or black, the general rule is that you should consume no more than 1,500 milligrams each day
- Exercising: At least 30 minutes of moderate activity 5 days per week can help you manage your weight, strengthen your heart, and manage your stress levels—all of which play an important role in controlling your blood pressure. Be sure to check with your healthcare professional before starting a new exercise program
- Lose weight, or maintain an ideal body weight: In one study over half of those overweight patients with mild (stage 1) hypertension, normalized their blood pressure with a 5% weight loss. The bottom line: It didn't take a whole lot of weight loss to help curb high blood pressure
- Limiting alcohol: Drinking too much alcohol can raise your blood pressure. In general, more than one drink a day for women and more than two for men is too many
- Taking your blood pressure medicine as prescribed: Put your prescription in your brief case or next to your toothbrush—whatever you need to do to remind yourself to take your medication and make it part of your routine
- Adopting healthier habits can seem daunting to some. But when it comes to lowering your blood pressure, there’s no easy way around steps like the ones above. On many occasions, I have had to reduce the amount of blood pressure medication that a patient is taking when they have made one or more of thes e lifestyle changes.
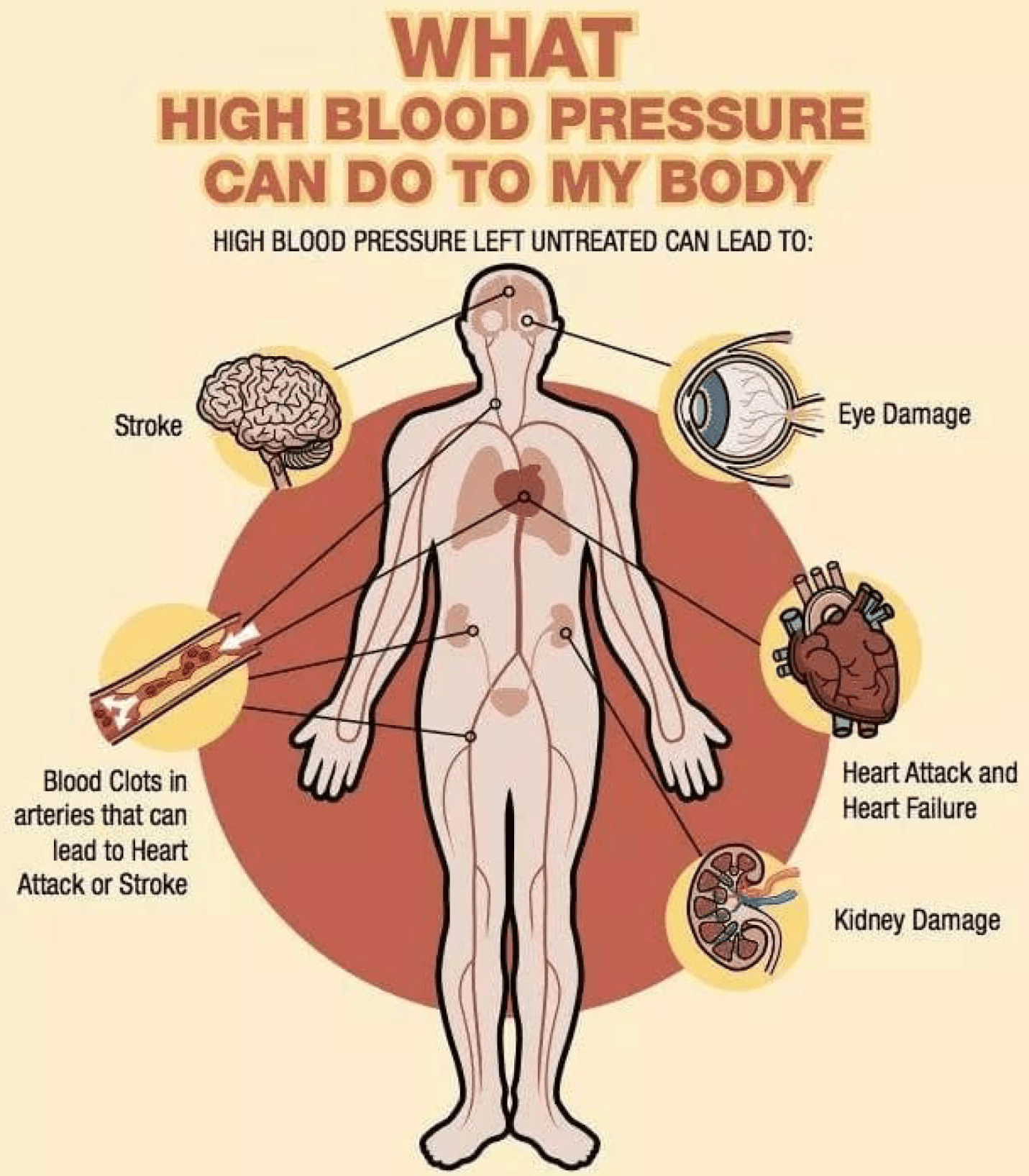


- 140/90 or higher is high blood pressure
- Between 120 and 139 for the top number, or between 80 and 89 for the bottom number is called prehypertension. Prehypertension means you may end up with high blood pressure, unless you take steps to prevent it.
Exercise and Physical Fitness
- Control your weight
- Lower your risk of heart disease
- Lower your risk for type 2 diabetes and metabolic syndrome
- Lower your risk of some cancers
- Strengthen your bones and muscles
- Improve your mental health and mood
- Improve your ability to do daily activities and prevent falls, if you're an older adult
- Increase your chances of living longer
Pregnancy
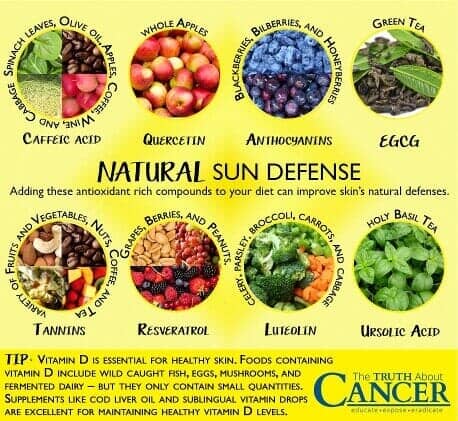
Skin Conditions
How To Prevent Skin Cancer

Prevention Tips:



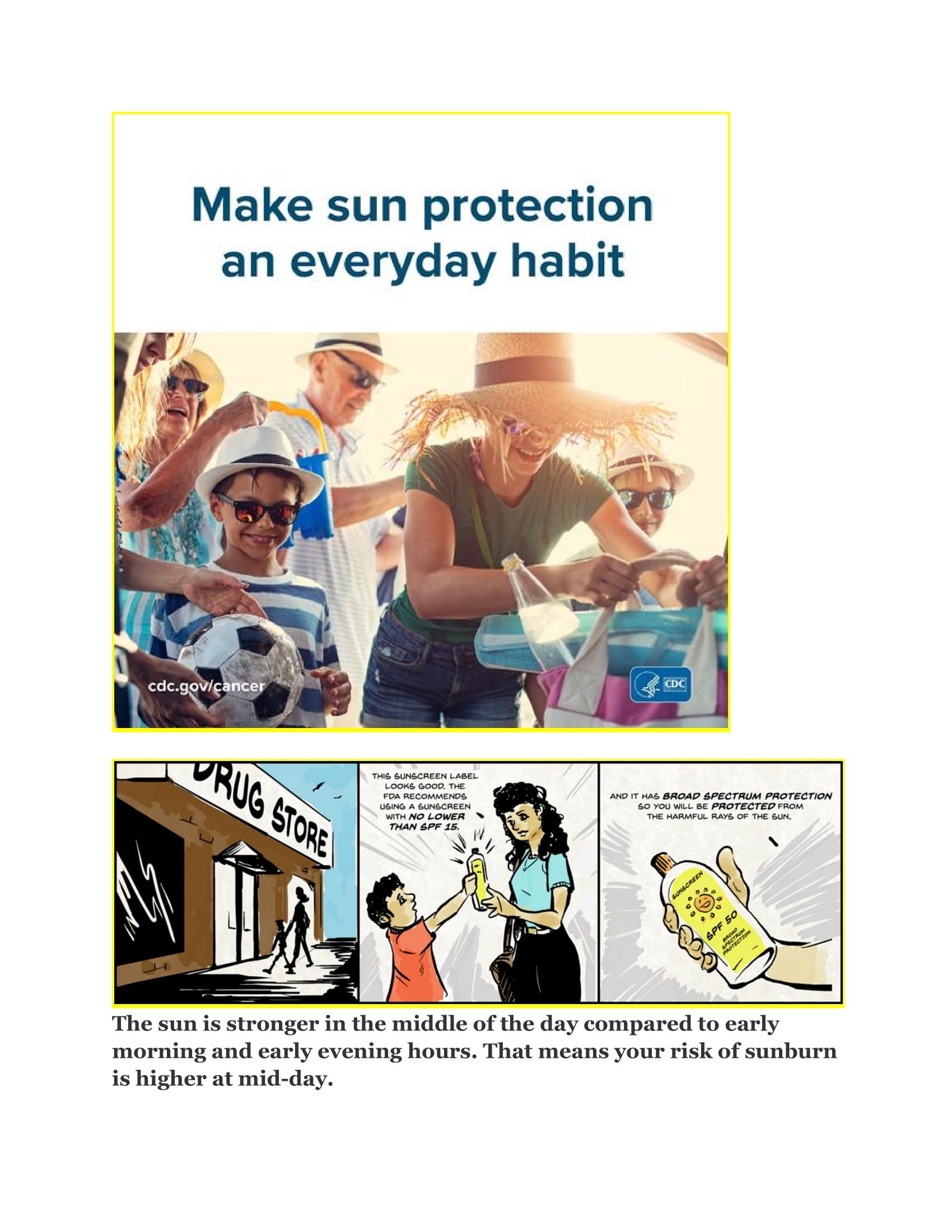
Sunburn First Aid:
Weight Control
- Choosing low-fat, low-calorie foods
- Eating smaller portions
- Drinking water instead of sugary drinks
- Being physically active
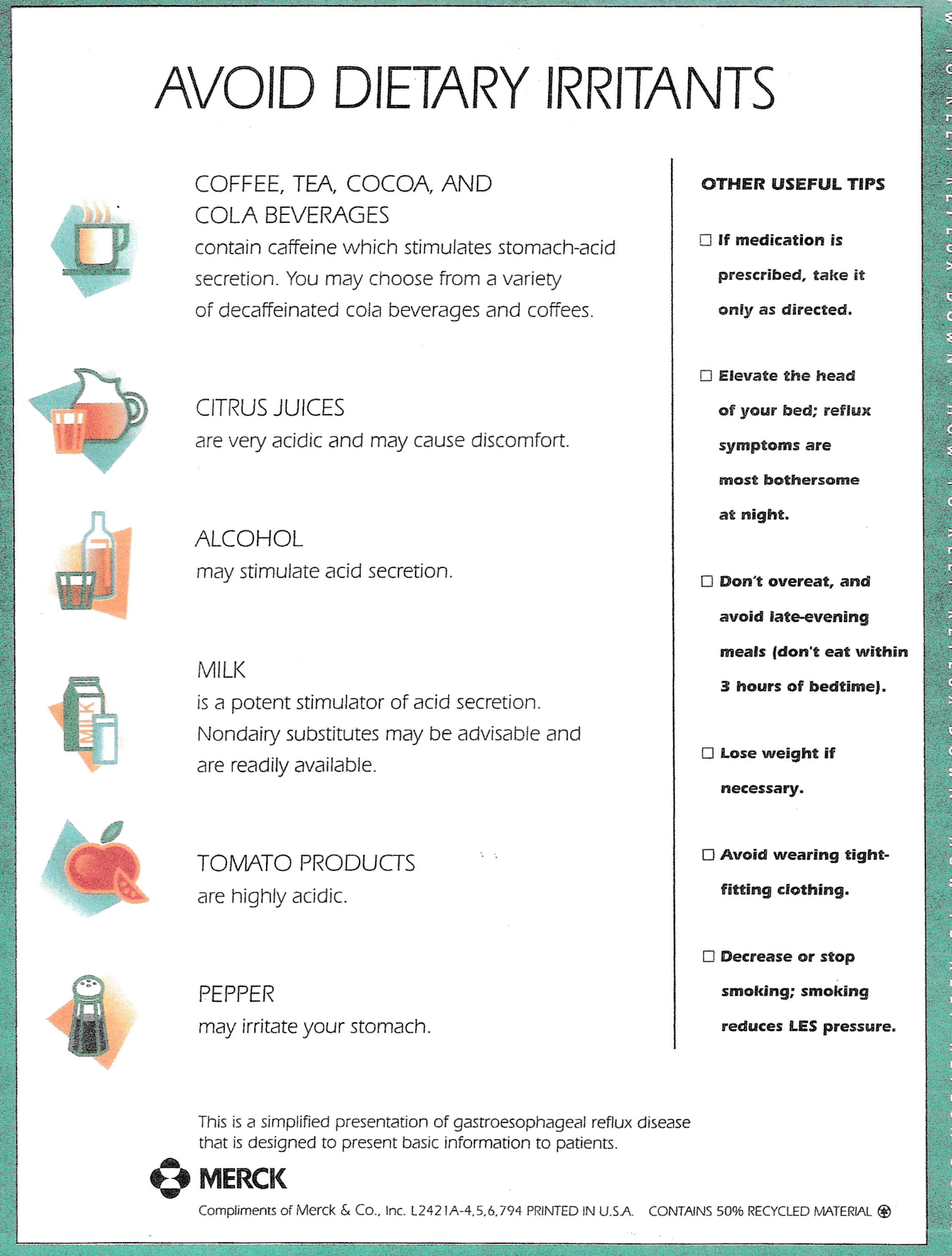
Reflux or GERD?
- Maintain a healthy weight.
- Eat smaller meals.
- Avoid triggering foods, including alcohol.
- Don't lie down for 3 hours after a meal
- Raise the head of your bed 6 to 8 inches by putting wood blocks under the bedposts.
- For an infant, try burping frequently during feeding. Keep the infant upright for 30 minutes after feeding.
- If you have reflux twice or more per week, see your health care provider
Acne
What is acne?
Acne is a very common skin condition identified by the presence of comedones (blackheads and whiteheads) and pus-filled spots (pustules). It usually starts during puberty. Acne ranges from a few spots on the face, neck, back and chest, which most teenagers will have at some time, to a more severe problem that may cause scarring and reduce self-confidence. For most, it tends to go away by the early to mid twenties, but it can go on for longer.
Your doctor may recommend a course of antibiotic tablets, usually erythromycin or a type of tetracycline, which is often taken in combination with a suitable topical treatment.
Antibiotics need to be taken for at least two months, and are usually continued until there is no further improvement. Typical courses last three to six months. Some should not be taken at the same time as food or can make your skin more sensitive to the sun, so read the instructions carefully. Here are some tips for looking after skin that has acne or is prone to it.
● Wash your face no more than twice each day with warm water and mild soap made for acne.
● Do not scrub the skin or burst the pimples, as this may push the infection further down, causing more blocking, swelling, and redness.
● Avoid popping pimples, as this makes scarring likelier.
● A specialist can treat a pimple that requires rapid removal for cosmetic reasons.
● Refrain from touching the face.
● Hold the telephone away from the face when talking, as it is likely to contain sebum and skin residue.
● Wash hands frequently, especially before applying lotions, creams, or makeup.
● Clean spectacles regularly as they collect sebum and skin residue.
● If acne is on the back, shoulders, or chest, try wearing loose clothing to let the skin breathe. Avoid tight garments, such as headbands, caps, and scarves, or wash them regularly if used.
● Choose makeup for sensitive skin and avoid oil-based products. Remove makeup before sleeping.
● Use an electric shaver or sharp safety razors when shaving. Soften the skin and beard with warm soapy water before applying shaving cream.
● Keep hair clean, as it collects sebum and skin residue. Avoid greasy hair products, such as those containing cocoa butter.
● Avoid excessive sun exposure, as it can cause the skin to produce more sebum. Several acne medications increase the risk of sunburn.
● Avoid anxiety and stress, as it can increase production of cortisol and adrenaline, which exacerbate acne. Try to keep cool and dry in hot and humid climates, to prevent sweating. Acne is a common problem. It can cause severe embarrassment, but treatment is available, and it is effective in many cases.
● ¿Qué es el acné?
● El acné es una afección cutánea muy común que se identifica por la presencia de comedones (puntos negros y puntos blancos) y manchas llenas de pus (pústulas). Por lo general, comienza durante la pubertad. El acné varía desde algunas manchas en la cara, el cuello, la espalda y el pecho, que la mayoría de los adolescentes tendrán en algún momento, hasta un problema más grave que puede causar cicatrices y reducir la confianza en sí mismos. Para la mayoría, tiende a desaparecer entre principios y mediados de los veinte, pero puede durar más tiempo.
● Su médico puede recomendarle un ciclo de tabletas de antibióticos, generalmente eritromicina o un tipo de tetraciclina, que a menudo se toma en combinación con un tratamiento tópico adecuado.
● Los antibióticos deben tomarse durante al menos dos meses y, por lo general, se continúan hasta que no haya más mejoría. Los cursos típicos duran de tres a seis meses. Algunos no deben tomarse al mismo tiempo que los alimentos o pueden hacer que su piel sea más sensible al sol, así que lea las instrucciones con atención. A continuación se ofrecen algunos consejos para cuidar la piel que tiene acné o es propensa a tenerlo.
● Lávese la cara no más de dos veces al día con agua tibia y un jabón suave elaborado especialmente para el acné.
● No frote la piel ni reviente los granos, ya que esto puede empujar la infección hacia abajo y causar más bloqueo, hinchazón y enrojecimiento. ● Evite las espinillas, ya que esto hace que las cicatrices sean más probables.
● Un especialista puede tratar una espinilla que requiera una rápida eliminación por motivos estéticos.
● Abstente de tocarte la cara.
● Mantenga el teléfono alejado de la cara cuando hable, ya que es probable que contenga sebo y residuos de piel.
● Lávese las manos con frecuencia, especialmente antes de aplicar lociones, cremas o maquillaje.
● Limpie las gafas con regularidad, ya que acumulan sebo y residuos cutáneos.
● Si el acné está en la espalda, los hombros o el pecho, intente usar ropa holgada para que la piel respire. Evite las prendas ajustadas, como cintas para la cabeza, gorras y bufandas, o lávelas con regularidad si las usa.
● Elija maquillaje para pieles sensibles y evite los productos a base de aceite. Quítese el maquillaje antes de dormir.
● Utilice una afeitadora eléctrica o navajas de seguridad afiladas al afeitarse. Suaviza la piel y la barba con agua tibia y jabón antes de aplicar la crema de afeitar.
● Mantenga el cabello limpio, ya que acumula sebo y residuos cutáneos. Evite los productos para el cabello grasos, como los que contienen manteca de cacao. ● Evite la exposición excesiva al sol, ya que puede hacer que la piel produzca más sebo. Varios medicamentos para el acné aumentan el riesgo de quemaduras solares.
● Evite la ansiedad y el estrés, ya que puede aumentar la producción de cortisol y adrenalina, que agravan el acné.
● Trate de mantenerse fresco y seco en climas cálidos y húmedos para evitar la sudoración. El acné es un problema común. Puede causar una gran vergüenza, pero hay tratamiento disponible y es efectivo en muchos casos.
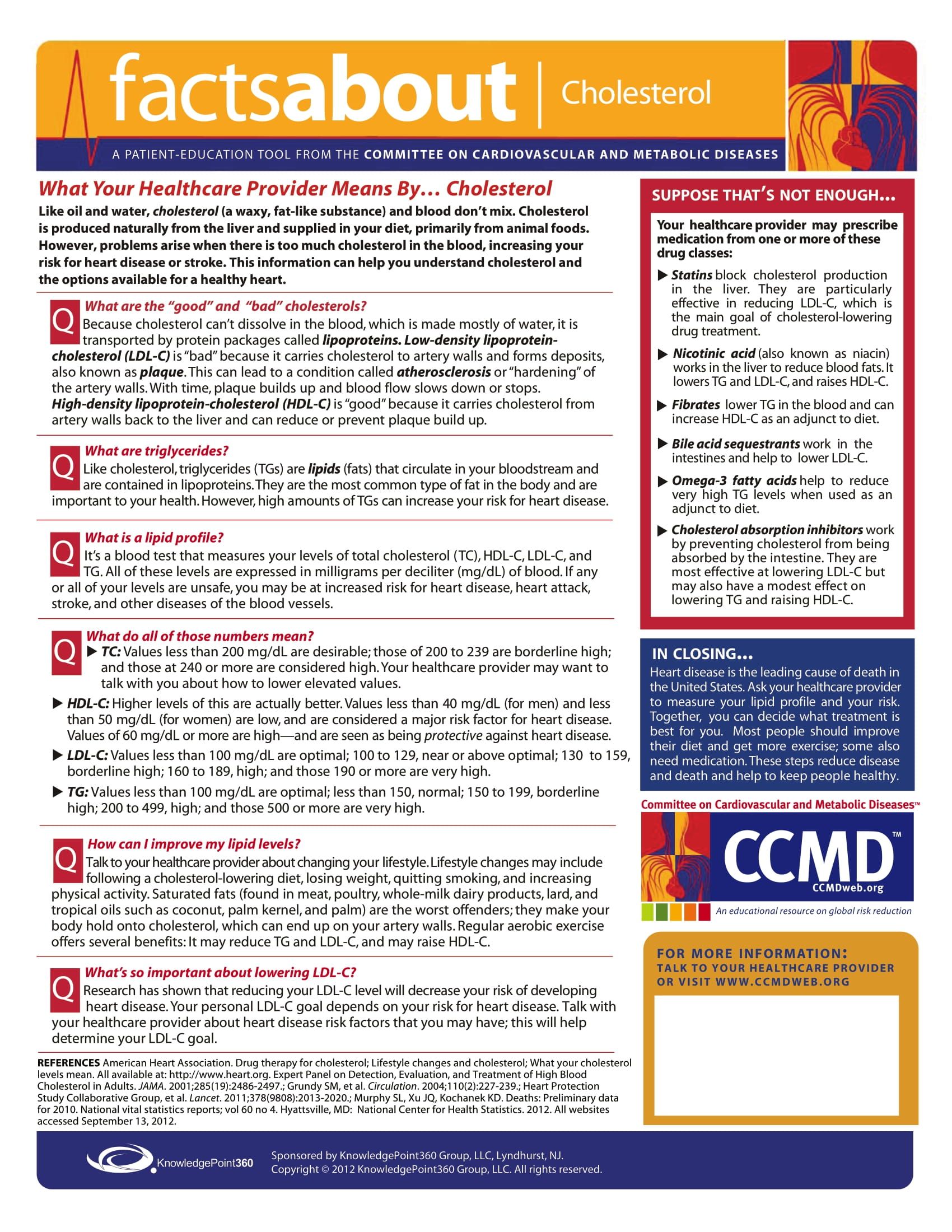
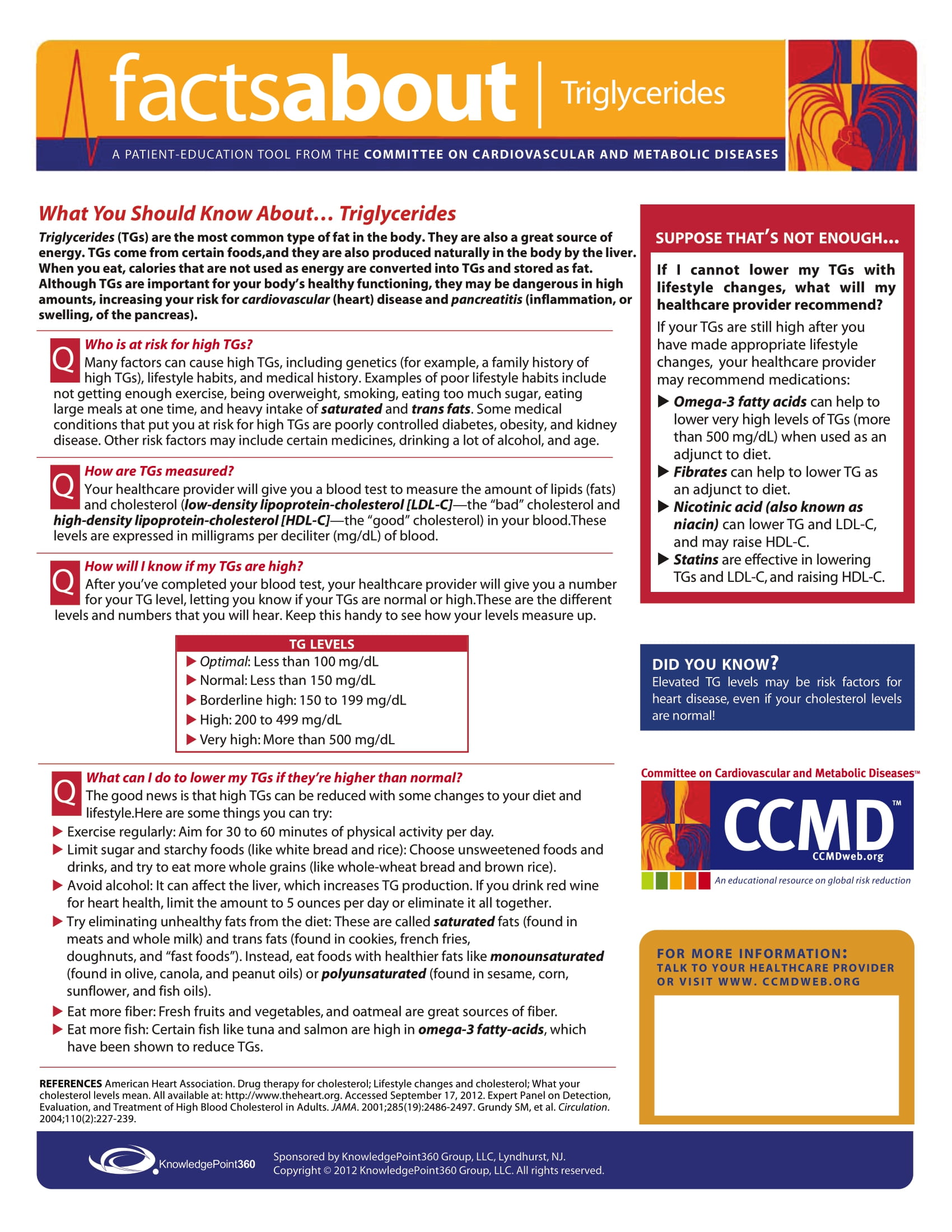
Cholesterol
Protect Yourself from Heart Attack and Stroke
Have you had your cholesterol checked? Most adults should have a cholesterol test every 4 to 6 years. That’s because nearly 78 million American adults have high levels of the type of cholesterol that’s linked to heart disease and stroke. Cholesterol is a waxy, fat-like substance that your body needs to function properly. It travels through your bloodstream to reach the cells that need it. Your cells use cholesterol for many important functions, like making hormones and digesting fatty foods. But too much cholesterol in your blood can cause waxy buildup called plaques in blood vessels. “These plaques can eventually become inflamed and rupture, leading to a clot,” explains cholesterol expert Dr. Ronald Krauss at UCSF Benioff Children’s Hospital Oakland. If a clot blocks blood flow through an artery in the heart, it can cause a heart attack. “Or, if this happens in the artery of the brain, it can cause a stroke,” he says. Cholesterol travels through the bloodstream in particles called lipoproteins. There are different types of lipoproteins that have different effects. Low-density lipoproteins, or LDLs, contribute to plaques. LDL cholesterol is sometimes called “bad” cholesterol. “Many people in this country have too many of these LDL particles in the blood,” Krauss says. Studies have found that lowering LDL cholesterol levels reduces heart disease and stroke. The most common cause of high LDL cholesterol is an unhealthy lifestyle. Excess body weight and eating a lot of animal fats are linked to high levels of LDL cholesterol. The genes that you inherit from your parents, other medical conditions, and certain medicines can also cause high cholesterol. You may also have heard about “good” cholesterol: high-density lipoproteins, or HDL. HDL particles absorb cholesterol and carry it to the liver. The liver then flushes it from the body. That’s why scientists previously thought that raising levels of HDL cholesterol might lower your risk for heart disease and stroke. But recent research suggests that HDL cholesterol works better in some people than others. And clinical trials haven’t found that medicines aimed at raising HDL cholesterol reduce the risk of heart attack. There’s still a lot to learn about HDL. Lab tests can measure the different types of cholesterol in your blood. How often you should get tested depends on your age and other risk factors, including a family history of high cholesterol or heart disease. If tests show that you have a high level of LDL cholesterol, your doctor may order additional tests. You can try to lower it by eating a heart-healthy diet, being physically active, and losing excess weight. For some people, lifestyle changes aren’t enough to lower LDL cholesterol. Your biological makeup can be a strong influence on cholesterol buildup, too. In these cases, a type of drug known as a statin is the usual treatment. Doctors may combine statins with other drugs. If your LDL cholesterol is very high, Krauss says it’s important that your family members get tested, too. If your genes put you at risk for high cholesterol, your close relatives might have a similar risk. Talk to your doctor about getting tested. And remember that heart-healthy lifestyle changes can not only lower cholesterol levels but also bring many long-term health benefits
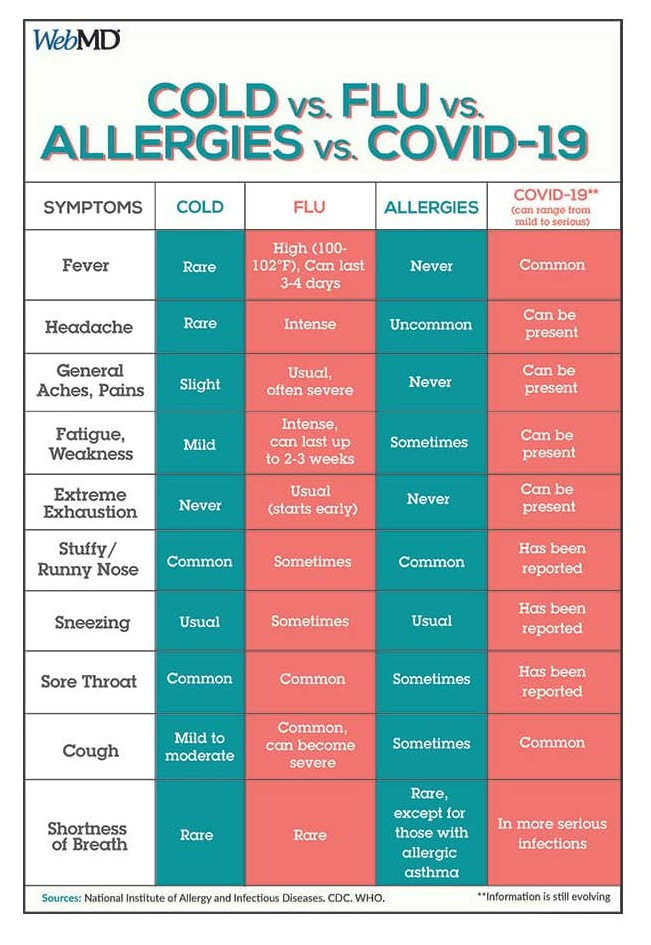
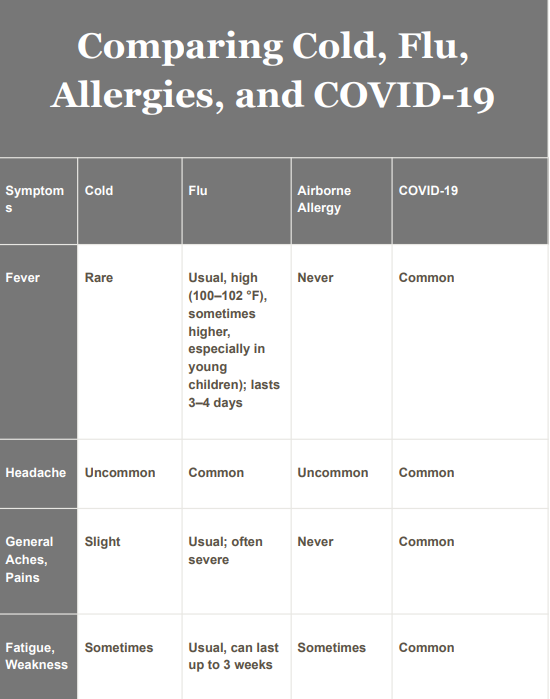
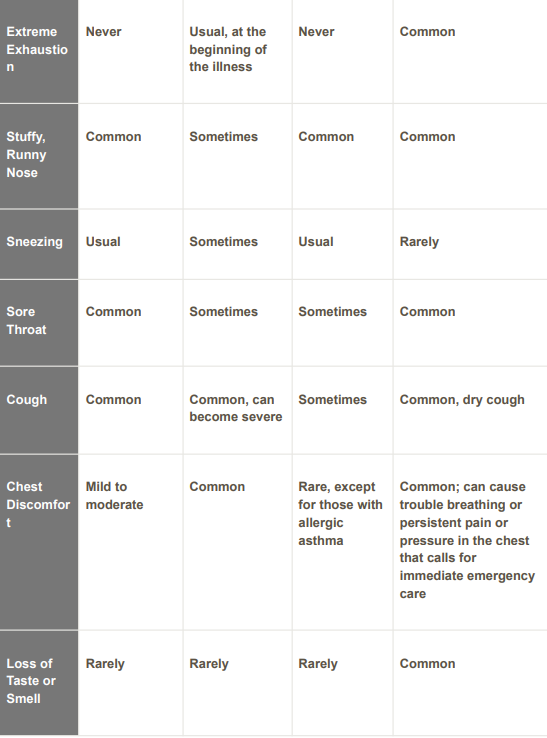
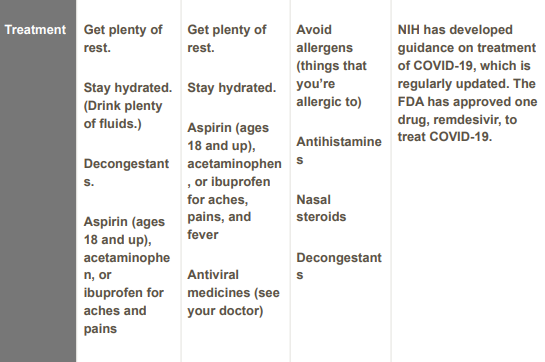
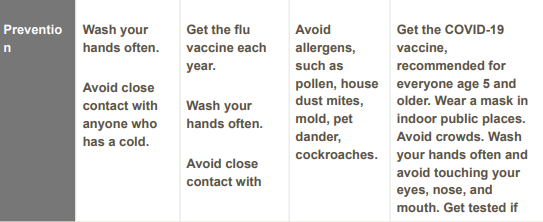
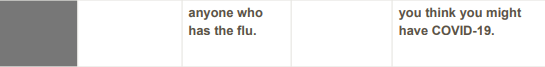
Flu, COVID-19, Allergies, or a Cold?
Staying Healthy This Winter

Feeling sick can be especially concerning these days. Could your sniffles be caused by COVID-19? Or the flu? A cold? Or maybe allergies?
Determining the cause of an illness can be tricky because many share some symptoms. They can leave you sniffling, coughing, and feeling tired. But there are important differences.
Figuring out what’s making you sick can help you recover and prevent spreading sickness to others.
Flu vs COVID-19
“Distinguishing COVID from flu can be difficult because the symptoms overlap so much,” explains Dr. Brooke Bozick, an NIH expert on respiratory diseases that affect the lungs.
Flu and COVID-19 are caused by different viruses that can be spread among people. Flu is caused by the influenza virus. COVID-19 is caused by SARS-CoV-2. Both can give you a fever, cough, headaches, and body aches.
Flu and COVID-19 also spread similarly. They’re transmitted by small particles that come from your nose and mouth when you sneeze, cough, sing, or talk, raising the possibility of infecting people who are nearby. Infected people may not have symptoms, but can still pass along either virus.
“Both influenza and COVID can be spread to other people before individuals develop symptoms,” notes Dr. Aubree Gordon, an infectious disease expert at the University of Michigan.
COVID-19 symptoms can take longer than flu symptoms to develop, she explains. Someone with flu usually has symptoms 1 to 4 days after being infected. A person with COVID-19 typically shows symptoms about 5 days after infection, although this can range from 2 to 14 days.
One telling sign of COVID-19 in some cases is loss of smell or taste. But because of other similar symptoms, there’s really only one way to be certain if you have COVID-19 or flu: Get tested.
“You can go and get a COVID test at many pharmacies, and your doctor can administer tests for flu,” Bozick says. COVID-19 tests are also available at many health centers. And you can buy testing kits approved for use at home.
Could It Be a Cold? Or Allergies?
Like flu and COVID-19, colds are also caused by viruses and can be passed to others.
Symptoms of a cold tend to be mild. You may have a runny nose, cough, congestion, and sore throat. But you won’t usually have the aches and fever that are common with COVID-19 and flu. Often, you’ll feel better in a couple of days.
There’s no cure for the common cold. Typical treatments include rest, fluids, and over-the-counter medicines. Some complementary treatments may help with cold symptoms, too. Taking honey may help with nighttime cough for children over 1 year old. Rinsing your nose and sinuses can help with congestion. You can use a neti pot or other nasal rinsing device. Be sure to only use water that’s been properly processed, such as distilled or boiled water, not tap water. Nasal rinses can bring relief for both cold and allergies.
Allergies can cause a runny nose and sneezing. But they’re not contagious. If your eyes, nose, or ears itch, that also could be an allergy.
Exposure to things like dust, pets, and tree or grass pollen can trigger allergies, which are caused by the immune system overreacting.
Allergy symptoms tend to stop when you’re no longer exposed to the cause. Unless you have asthma, allergies typically do not cause breathing problems. Allergies can be treated with drugs like antihistamines, decongestants, and nasal steroids.
Wintery Mix of Viruses
Winter is the prime cold and flu season. You’re more likely to be indoors and closer to others when it’s colder outside. Weather also plays a role in the spread of viruses.
“Cold and flu viruses survive better and are more transmissible if it’s cooler and if there’s lower humidity,” Gordon explains.
Experts are concerned that flu and COVID-19 cases may increase and overlap in the winter. Flu cases usually start to increase around October and peak between December and February. Being infected with flu and SARS-CoV-2 at the same time is possible, as is showing symptoms of both.
If you’re sick with the flu, your doctor may prescribe antiviral drugs. Such drugs can make your flu milder and shorten the time you are sick. They work best if they’re used early in your illness.
The FDA has also approved one antiviral drug, called remdesivir, to treat COVID-19. Other treatments are in development and under review. No complementary approaches have been shown to be helpful for fighting off flu or COVID-19.
Fortunately, strategies to prevent the spread of COVID-19 also prevent the spread of flu and cold. “Measures like masking and social distancing work for other respiratory viruses, as well as COVID-19,” says Dr. Chip Walter, who studies vaccine development at Duke University.
Staying Well
There’s another really important way to fight viruses. “Get your flu shot and COVID-19 vaccine,” Walter advises. They are safe and effective ways to protect yourself and those around you.
Don’t forget to vaccinate your children, too. That is the best way to protect their health. COVID-19 vaccines are now recommended for everyone age 5 years and older. Flu vaccines are recommended for everyone 6 months and older.
Flu vaccines are designed to protect against the four types of flu viruses that scientists expect to circulate that year.
Researchers like Walter and others are working to develop flu vaccines that last longer and offer broader protection against many flu strains.
Masks continue to be an important tool for stopping the spread of respiratory viruses, such as COVID-19. “With the pandemic still ongoing, it’s going to be really important that people wear masks,” Gordon says. Try to avoid crowded indoor situations when possible, too.
For more tips on guarding against getting sick this winter, see the Wise Choices box.
Face Masks and COVID-19
Protecting Yourself and Others

To fight the spread of COVID-19, many places now require people to wear face masks. But the advice on wearing them has changed over the course of the pandemic. This has led some people to question: Do face masks even protect against COVID-19?
“Yes, absolutely,” says Dr. Adriaan Bax, a biophysicist at NIH. He has been testing how well different types of masks work. Masks, he explains, can help stop the spread of COVID-19 for a few reasons.
First, masks can trap fluid droplets that exit the mouth while you’re speaking. If you have COVID-19, these droplets contain virus that can be inhaled by others.
Bax and his colleagues have shown that just by talking, a person produces thousands of these little droplets every second. Speaking loudly or singing produces even more droplets.
Stopping droplets at the source is the easiest way to prevent the virus from spreading through the air. Wearing a mask can play a crucial role. Bax and colleagues have found that even a simple cloth mask can stop nearly all droplets produced during speech.
After droplets leave someone’s mouth, the water in them quickly evaporates. This causes the droplets to shrink. These shrunken droplets are called aerosols. They can float in the air for anywhere from minutes to hours. Once the virus is carried in such tiny aerosols, it becomes more difficult to stop.
Masks can also help protect the people wearing them. Studies have found that NIOSH-approved N95 respirators and KN95 masks block aerosols from entering the airway very effectively.* Surgical and cloth masks are less effective, but they still provide some protection. How well they work depends on the number of layers, choice of materials, and whether they’re worn properly.
Even if a mask doesn’t block all of the aerosols, it may still protect the wearer against severe disease. Severe COVID-19 tends to occur when virus gets into the lower airway and the lungs.
Wearing a mask may help the body clear out virus from the lower airway before it reaches the lungs. This is because, as Bax’s team has shown, wearing a mask traps the moisture that would otherwise escape when you exhale. This raises the amount of moisture in your airways (or the humidity).
Moisture is essential to promote the natural clearance process of the airways. This helps keep the lungs free of contamination by dust, pollutants, and viruses. Masks may aid this process by raising the humidity.
“Some may find wearing a mask uncomfortable, especially on hot and humid days. This is largely because of the humidifying effect. But this drawback is very minor compared to the benefit that masks offer,” says Bax.
For most people, cloth masks and surgical masks don’t interfere with normal breathing. Oxygen and carbon dioxide are much smaller than the respiratory droplets that carry the virus and pass easily through masks.
Masks work best when we all wear them. But with any mask, not all virus particles are blocked. That’s why it’s still important to stay a distance from others, generally about six feet. For tips on wearing masks, see the Wise Choices box.
And remember: Getting a COVID-19 vaccine is the best way to protect yourself and others from the virus.

HIV and AIDS: Know the Facts
Treatments Work, but Prevention Is Key

It’s been more than 30 years since a disease now called AIDS was first recognized in the United States. Back then, it was considered a death sentence. No treatments were available, its cause was unknown, and people often died within a few months after being diagnosed. Today, people infected with HIV—the virus that causes AIDS—can live full, healthy lives, in large part because of medicines and other discoveries made with NIH support.
The terms HIV and AIDS can be confusing, because they’re related but different. HIV is a virus that harms your immune system by invading and then destroying your infection-fighting white blood cells. AIDS is the final stage of an untreated HIV infection. People with AIDS can have a range of symptoms, because their weakened immune systems put them at risk for life-threatening infections and cancers.
HIV virus passes from one person to another through certain body fluids, such as blood and semen. About 90% of new HIV infections in the U.S. occur during sex. Shared needles and injection drug use is the second most common route of infection. HIV can also spread from an infected mother to her newborn. HIV isn’t spread through casual contact, such as shaking hands, hugging, sneezing, sharing utensils, or using bathrooms.
Today, by taking a combination of HIV-fighting medicines (called antiretroviral therapy), fewer Americans with HIV are developing AIDS. And some HIV infections can now be prevented by taking daily medications (called PrEP).
Because of these advances, some people may think that there’s little need to be concerned about HIV and AIDS. But nothing could be further from the truth. Nationwide, more than 1 million people are infected with HIV, and each year over 50,000 more become newly infected. About 1 in 7 Americans who have HIV don’t even realize they’re infected, so they may be unknowingly spreading the virus to others. The problem is even more severe in developing nations, especially in parts of Africa.
Even though treatments and prevention strategies can keep HIV in check, there’s still no cure and no vaccine to prevent HIV infections. That’s why NIH-funded scientists continue to search for new, more effective ways to halt HIV infections.
“If you get a diagnosis of HIV infection, and you begin antiretroviral therapy in a timely fashion, before your immune system becomes substantially compromised, your prognosis is excellent,” says Dr. Anthony S. Fauci, NIH’s infectious disease chief, who first began treating AIDS patients in the early 1980s. Studies show that with early treatment, HIV levels may become so low that the virus becomes undetectable in the blood. That lengthens life and reduces the risk of spreading HIV to others. “If those who are infected stay on therapy, they can save their own lives and also help keep HIV from infecting their sexual partners,” Fauci says.
Keeping HIV infections in check requires early diagnosis and taking daily HIV medications for life. Even if it’s undetectable in the blood, once a person’s been infected with HIV, it remains forever hidden in the body. “HIV has the ability to integrate itself into your cells and hide in an inactive form, called a reservoir,” says Fauci. Although medicines can keep virus levels low, they don’t clear out the viral reservoir. So if treatment lapses, HIV comes out of hiding and rushes back into the bloodstream.
For some people, keeping up with this daily health regimen can be a challenge. Nationwide, fewer than 1 in 3 people with HIV takes antiretroviral medicines regularly enough to reduce the virus to undetectable levels. That’s why ongoing NIH-funded studies are creating and evaluating medications that might be taken less often, such as once a month. This approach will be tested in a large clinical trial expected to begin in Africa later this year. Other approaches that don’t depend on daily anti-HIV drugs are also being tested.
Research over the past few decades has identified preventive strategies that work: limit your number of sexual partners, never share needles, and use condoms correctly and regularly. NIH is also exploring new ways to prevent HIV infections, including experimental vaccines.
One preventive approach for people at increased risk for HIV infection involves taking a daily dose of an antiretroviral drug. “In terms of prevention, a game-changer that we’ve got right now is pre-exposure prophylaxis, or PrEP,” says Dr. Carl W. Dieffenbach, who heads NIH’s global research efforts in HIV/AIDS. “This strategy protects you from getting infected with HIV if you take the medication daily.”
A pill form of PrEP (called Truvada) is approved by the U.S. Food and Drug Administration for people at high risk of getting HIV. Truvada combines 2 antiretroviral drugs already used to treat HIV infections.
When it comes to treatment and prevention, Dieffenbach says, “the most important activity that you can engage in is first getting an HIV test.” Your health care provider, community health clinic, and others may offer quick HIV tests, often at no cost to you. The U.S. Centers for Disease Control and Prevention recommends at least a yearly HIV screening for people considered at high risk for infection. Testing is especially important for young people from ages 13 to 24, because more than half in that age group who tested positive for HIV didn’t know they’d been infected.
Some people avoid getting tested because they’re afraid of the possibility of being HIV-positive. Others may feel embarrassed or uncomfortable talking about sexual issues, and so they don’t get tested. But the earlier HIV is diagnosed and treated, the better the outcome.
“The stigma associated with HIV infection makes it difficult for some people who are at risk to come forward and either be counseled about how to avoid infection, or if they are infected, to get into a health care system and stay in the health care system,” Fauci says. But studies show that open communication can help people treat and prevent HIV.
“The stigma problem can only be solved one person or one family at a time, because each person’s situation is unique,” Dieffenbach says. “It’s about continuing a conversation with openness and acceptance in communities. As hard as that is, it does really matter."
Herpes
Genital Herpes Often Unrecognized

It’s an uncomfortable topic, but it’s a health issue you should know about. Nationwide, about 1 out of 6 people between ages 14 and 49 is infected with the herpes simplex virus type 2—the main cause of genital herpes. Surprisingly, most people don’t know they’re infected. Even if you have no symptoms, or only mild ones, you can still transmit the virus to others.
Herpes simplex virus (HSV) comes in 2 forms. The most common, HSV-1, is best known for causing cold sores or fever blisters on the face, especially on the lips and mouth. But HSV-1 can also cause genital herpes. HSV-2 usually affects the genitals, but can also infect the mouth. Both types of HSV can pass from one person to another through sexual or other skin-to-skin contact.
“Once people are infected with herpes simplex, the virus stays in the body for the rest of their lives,” says Dr. Carolyn Deal, who heads the sexually transmitted diseases branch at NIH. Symptoms may first appear about 2 weeks after infection. After that, the herpes virus goes into hiding in your nerve cells. It may re-emerge several times a year. Over time, reappearances occur less often.
The first outbreak is usually the most severe and lasts the longest, sometimes 2 to 4 weeks. During an outbreak, you might notice tingling or sores (lesions) near the area where HSV first entered your body. Small red bumps are the first to appear. They change into small blisters, and then become itchy, painful sores that might develop a crust. The sores eventually heal without leaving a scar.
Often, though, people don’t recognize their first genital herpes outbreak or later recurrences. A study by the U.S. Centers for Disease Control and Prevention found that more than 80% of people with HSV-2 infections have not been diagnosed with the disease.
Your health care provider can sometimes diagnose genital herpes by looking at the sores or testing a sample from infected skin. Between outbreaks, a blood test can detect evidence of HSV-1 or HSV-2.
Although there’s no cure for herpes, prescription medicines can help calm symptoms and prevent future outbreaks. Taken regularly, these medications can also reduce the risk of passing herpes to sexual partners.
“For prevention, the recommendations for genital herpes are similar to many other sexually transmitted diseases,” says Deal. The most reliable way to prevent infection is to abstain from sex or to be in a long-term monogamous relationship with an uninfected partner. Condoms can also reduce the risk of transmission, but are not a reliable solution, as they may not cover all infected areas. Infected people should avoid having sex with uninfected partners during an outbreak.
Although herpes infections generally don’t cause serious medical problems alone, they can cause complications. Genital herpes can increase your chances of becoming infected with HIV, the virus that causes AIDS. In rare cases, herpes outbreaks during pregnancy can put the newborn child at risk for serious or even deadly infections.
Although genital herpes is a lifelong disease, there are many options for managing the condition and preventing its spread. Talk to your health care
Herpes infections are caused by herpes simplex virus (HSV) types 1 and 2. These viruses are contagious and transmitted from one person to another through skin-to-skin contact. Kissing or touching is the main cause of HSV-1 transmission, and sexual contact is the main cause of HSV-2 transmission Genital herpes is a common sexually transmitted disease (STD) that any sexually active person can get. Most people with the virus don't have symptoms. Even without signs of the disease, herpes can still be spread to sex partners.
Genital herpes cannot be cured, but outbreaks can be treated. Your doctor can give you medicines to make the sores go away more quickly and to reduce the number of outbreaks. When you have herpes sores, you should wear loose clothing and keep the genital area clean and dry. Try not to touch the sores. If you do touch them, wash your hands with soap and water right away because the virus can be passed with your fingers.People who have herpes can pass the virus from oral or genital contact even when they do not have sores. Males should use latex condoms every time they have sex to lower the risk of getting genital herpes. However, it does not completely remove the risk. You should not have sex with someone who has active sores, even with a condom. Ask your partner if he or she has ever had a herpes infection. If your partner has had herpes, you should see your doctor for information to help prevent you from getting it. Do not have oral sex, kiss, or share cups, glasses, or lip balm with someone who currently has, or has recently had, cold sores.
Las infecciones por herpes son causadas por el virus del herpes simple (HSV) tipos 1 y 2. Estos virus son contagiosos y se transmiten de una persona a otra a través del contacto de piel a piel. Besar o tocar es la principal causa de transmisión de HSV-1, y el contacto sexual es la principal causa de transmisión de HSV-2 El herpes genital es una enfermedad de transmisión sexual (ETS) común que puede contraer cualquier persona sexualmente activa. La mayoría de las personas con el virus no presentan síntomas. Incluso sin signos de la enfermedad, el herpes se puede transmitir a las parejas sexuales. El herpes genital no se puede curar, pero los brotes se pueden tratar. Su médico puede darle medicamentos para que las llagas desaparezcan más rápidamente y para reducir la cantidad de brotes. Cuando tenga llagas de herpes, debe usar ropa holgada y mantener el área genital limpia y seca. Trate de no tocar las llagas. Si los toca, lávese las manos con agua y jabón de inmediato porque el virus se puede transmitir con los dedos. Las personas que tienen herpes pueden transmitir el virus por contacto oral o genital incluso cuando no tienen llagas. Los hombres deben usar condones de látex cada vez que tengan relaciones sexuales para reducir el riesgo de contraer herpes genital. Sin embargo, no elimina completamente el riesgo. No debe tener relaciones sexuales con alguien que tenga llagas activas, ni siquiera con condón. Pregúntele a su pareja si alguna vez ha tenido una infección por herpes. Si su pareja ha tenido herpes, debe consultar a su médico para obtener información que ayude a prevenir que lo contraiga. No tenga sexo oral, no bese ni comparta tazas, vasos o bálsamo labial con alguien que actualmente tenga, o haya tenido recientemente, herpes labial.
Flu: Get Vaccinated
Influenza, or flu, can knock you off your feet and leave you miserable for nearly a week. It can cause fever, aches and pains, coughing, and exhaustion.
The best way to avoid this fate is to get a flu vaccine each year as early as possible, before or even during flu season, which usually lasts from October to as late as May. The vaccine is available as either a shot or a nasal spray.
Flu is highly contagious. When infected people cough or sneeze, the flu virus can spread to others up to 6 feet away. As many as 1 in 5 Americans come down with the flu each year, and kids are 2 to 3 times more likely than adults to get sick with the flu. Most cases are mild, but flu can also be serious, leading to hospitalization and even death.
Flu vaccines can reduce illness, doctors’ visits, and missed work and school. Vaccines can also prevent flu-related hospitalizations and deaths. When more people get vaccinated, it’s harder for the flu virus to spread.
Experts recommend that everyone 6 months and older get the annual flu vaccine, with rare exceptions. Talk to your doctor if you have questions about which vaccine options are best for you and your family. Learn more at www.flu.gov
COPD
Living With Chronic Obstructive Pulmonary Disease

Maybe you’ve noticed that you get out of breath doing light activities lately. Or have a cough that won’t go away. You might think it’s temporary, or just part of getting older.
But these issues can also be signs of chronic obstructive pulmonary disease, more commonly called COPD. With COPD, your lungs can no longer take in all the air you need.
More than 16 million people in the U.S. are living with COPD. Millions more likely have the disease but don’t know it. Symptoms can be mild at first and get worse over time.
“Some people with COPD get very short of breath when they try to walk, or do any kind of physical activity,” says Dr. Janet Larson, who studies COPD at the University of Michigan. “Some are bothered by persistent coughing.”
People may also feel tightness in their chest, experience wheezing, or a whistling or squeaky sound when breathing. They can also feel extremely tired, or fatigued.
“But many people don’t recognize the symptoms, or don’t know they can be from a disease,” says Dr. Prescott Woodruff, a lung specialist at the University of California, San Francisco.
COPD includes two main conditions. In one, called emphysema, tissue inside the lungs breaks down. In the other, called chronic bronchitis, the airways are irritated and show signs of inflammation. Many people with COPD have both.
“There are many things we can do for COPD,” Woodruff says. “Most of them can improve your quality of life. And some of them can improve life expectancy. So we want people to recognize the symptoms and seek help.”
Lessening Lung Irritation
Smoking is the main risk factor for the disease. But up to a quarter of people who develop COPD have never smoked.
The number of people in the U.S. who smoke has dropped over the last few decades. “But the amount of chronic lung disease has not declined as fast as we would have expected, given the decrease in smoking,” says Dr. Joel Kaufman, who studies how the environment impacts chronic diseases at the University of Washington.
Other factors can also play a role. Second-hand smoke—smoke in the air from other people smoking—is a risk factor. Others include your age, gender, and where you live and work.
COPD is more common in women and in people over the age of 40. People with a rare genetic disorder, called AAT deficiency, are also at increased risk.
COPD is also about twice as common in rural communities compared with urban ones. That’s largely because these communities have higher smoking rates.
Long-term exposures to other substances, including some types of chemical fumes and dust, may also increase the risk of COPD.
In a recent study, Kaufman and his team found that people who lived in areas with high air pollution had more emphysema-like changes in their lungs over time. This highlights additional risk factors that can potentially be lowered for whole communities, Kaufman explains.
“The more we understand about these risks, the more we can effectively target air quality improvements going forward,” says Kaufman.
Boosting Quality of Life
People who currently smoke or smoked in the past may feel stigmatized and embarrassed to talk with their doctor, when they shouldn’t, Woodruff says. “That’s a huge population that may not be getting the attention they need,” he says.
If you have symptoms of COPD, talk with your health care provider. They can refer you for testing. The main test used to diagnose COPD is called spirometry. In this test, you blow into a tube connected to a small machine. The machine measures how well your lungs are working.
Some people may also need imaging or blood tests. These tests can help determine whether their COPD is severe. They may also rule out other possible causes of symptoms.
Treatments for COPD can’t yet cure the disease. But they can slow the rate at which it gets worse, and make you feel better. Medications can help some people breathe more easily. These include drugs that help open the airways or reduce inflammation.
People with severe COPD may need oxygen therapy. Some may eventually have surgery. But usually only as a last resort if they don’t improve from taking medicines.
Pulmonary rehabilitation can also be used to treat the condition. These programs help you learn new breathing strategies, improve your body’s endurance and strength, and move in ways that preserve your energy. They may also include mental health care and nutrition counseling.
“People with COPD tend to be some of the least physically active people,” says Larson. Many feel embarrassed that they can’t keep up with other people, she explains. This can lead them to avoid activities they used to enjoy.
Larson and her team are testing a program to build light physical activity into the daily lives of people with COPD. Light physical activity—such as walking and using bands for strength exercises—can improve their health and energy levels, she explains.
By making exercise more accessible, “we hope that if they have a flare-up of their disease, and have to quit being active for a while, that they’ll be able to get right back to it on their own,” Larson says.
In an early study of the program, people with COPD increased their activity levels by more than half an hour a day. Talk with your health care provider to learn more about rehab programs.
Personalizing Treatments
Better treatments are still needed for COPD. Scientists first need to learn more about how the disease differs between people.
“By identifying the different subtypes of COPD, we can then target the specific underlying problems with new therapies,” Woodruff says.
In a recent study, Woodruff’s team identified one such subtype. They found that many current or former smokers had normal results on a spirometry test, but still had other symptoms of COPD, like a chronic cough or trouble breathing.
The researchers are now testing whether COPD drugs can help people with this subtype feel better and prevent them from developing full-blown COPD.
The team also found that some people with COPD have a type of inflammation in their lungs that looks like asthma. This may be another subtype of COPD. Now they’re testing whether asthma medications can help reduce symptoms in these patients.
For now, lifestyle changes and medications can help people with COPD manage symptoms. See the Wise Choices box for tips to help you breathe better
Pregnancy Check-Ups
Healthy Start for Mom and Baby

Life is busy before a baby arrives. There are many things to do to prepare. One of the most important is to visit your health care provider regularly.
Check-ups before your baby is born are called prenatal visits. They help make sure you and your baby are healthy. Your health care provider will look for certain problems that can happen during pregnancy. Some issues are best treated early. Others can be prevented before they start.
“Prenatal care is fundamental for shaping the lives of women and their children,” says Dr. Monica Longo, an NIH expert on prenatal health. Longo cares for women with high-risk pregnancies. Such women have a higher chance of complications.
If you think you may be pregnant, schedule a visit with your provider. If you’re pregnant, you’ll need to start regular prenatal visits. Most women have check-ups about once a month in the beginning. Then, they go more often later in the pregnancy.
During a prenatal visit, your provider will ask about your health history. They will also perform a physical exam and weight check. They’ll let you know how much weight gain is healthy for your body and help track your progress.
You’ll also be asked to provide a urine sample. Urinary tract infections (UTIs) are common during pregnancy. UTIs and other infections increase the risk of having a preterm birth. This is when you give birth at 37 weeks or earlier.
“One of the primary purposes of prenatal care is actually prevention,” says Longo. “We screen women to find potential health problems before those issues can worsen.”
During certain stages of pregnancy, your provider will perform blood tests and imaging tests. These include ultrasound exams to look at the baby’s growth and development. Visits are also an opportunity to talk with your provider about how to give your baby a healthy start.
“During prenatal visits, we educ-ate and counsel moms about healthy habits, healthy food choices, and exercise,” Longo says. “We also address any concerns a new mom-to-be might have.”
Taking a prenatal vitamin is also key. Folic acid is included in most prenatal vitamins. It reduces the risk of severe birth defects that affect the developing brain and spine.
It’s important to stay away from things that could harm your baby. These include certain medications, smoking, and alcoholic drinks. Also, talk with your provider about any health conditions. Conditions like diabetes (a disease that causes high blood sugar) and high blood pressure need to be brought under control.
Some women choose to talk with their provider before becoming pregnant. This is called a preconception visit. It can help you plan for a safer pregnancy.
Early and regular care for you and your developing baby is important. Studies show that prenatal care reduces the risk of having a low-birth weight baby. Low birth weight can cause health problems. Even during the pandemic, it’s essential to keep up with regular prenatal care.
“Providers around the globe have adapted prenatal care to fit the current challenges,” says Longo. That means using telehealth for visits that don’t have to be done in person.
Health care providers are also seeing fewer patients and extending the time between them. This reduces possible exposure in waiting rooms
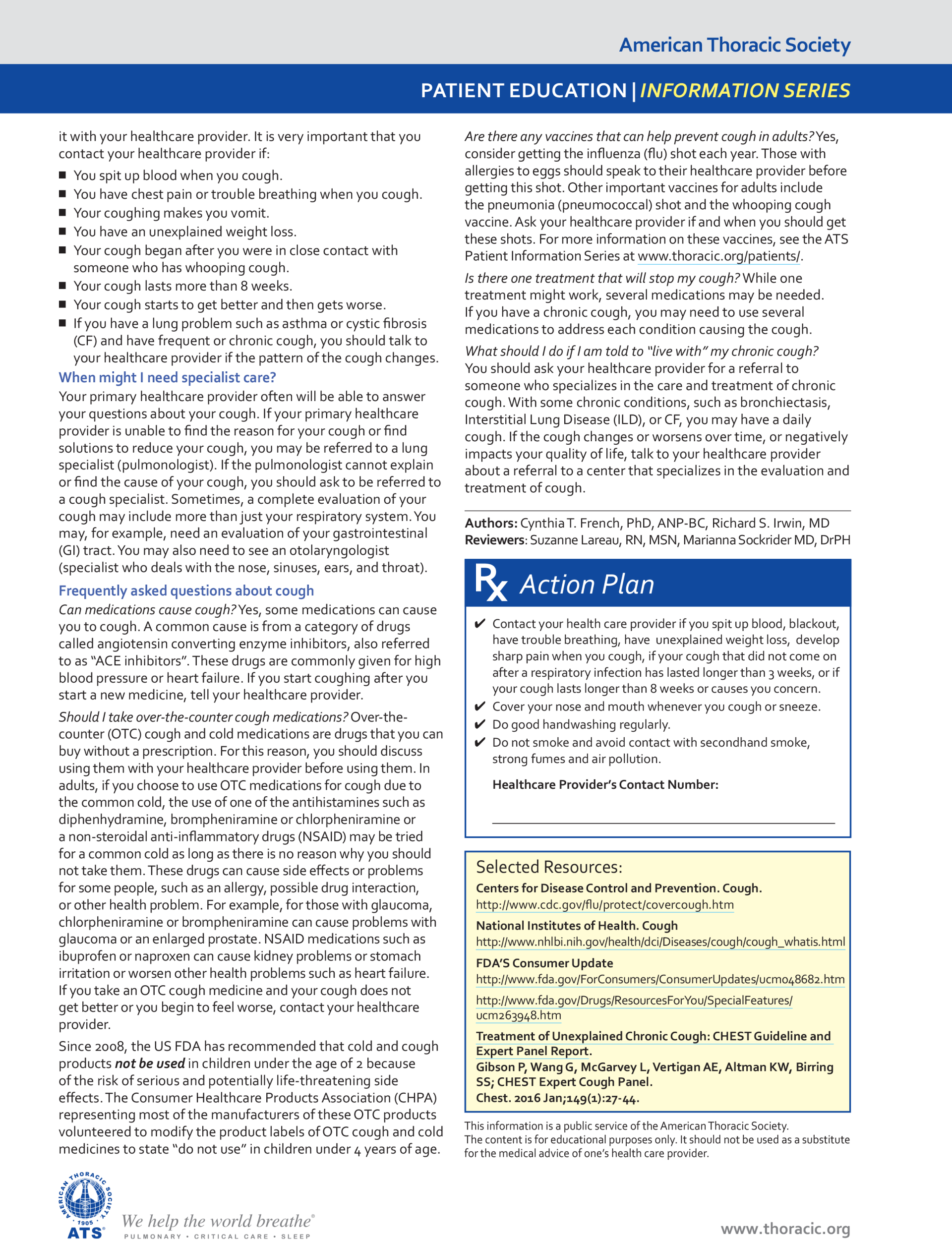
Managing Asthma
Learn To Breathe Easier

Most people have little trouble climbing a flight of stairs or taking a brisk walk, but these simple activities can be tough for someone with asthma. Although there’s no cure, you can breathe easier by knowing how to keep the condition under control.
Asthma is a common, long-lasting disease that affects the lungs. It can begin in childhood or adulthood. More than 25 million Americans have asthma, including 7 million children. Without proper care, asthma can become serious, even deadly. But most people with asthma learn to manage the disease so they have few symptoms or none at all.
Major symptoms of asthma include wheezing (a whistling sound when breathing), shortness of breath, coughing that’s worse at night and early morning, and chest tightness. These symptoms arise from reactions that narrow the airways, the tubes that carry air into and out of your lungs. When symptoms flare up, it’s called an asthma attack.
The airways of people with asthma are prone to inflammation, which causes the airways to swell and narrow. They become extra sensitive to certain substances that are breathed in. These are called “triggers.”
Asthma triggers can worsen inflammation and cause the muscles around the airways to tighten, further shrinking air passages and making it harder to breathe. Cells in the airways might also produce excess mucus (a sticky, thick liquid), making the airways even narrower.
Common asthma triggers include cigarette smoke, air pollution, mold, house dust mites, and furry animal dander. Other asthma triggers include weather changes, exercise, stress, and respiratory infections like common colds.
“Preventing such infections is important,” stresses Dr. Stewart Levine, an asthma expert at NIH. “People who have asthma should also obtain a flu shot, as they may be at higher risk for flu-related complications.”
Asthma is one of the most common causes of chronic (long-term) illness in children—and some symptoms appear more often in children than in adults. “Children have smaller airways, so if they have asthma, they tend to wheeze more often, particularly during the night,” says Dr. Robert Lemanske, Jr., a pediatric asthma expert at the University of Wisconsin.
Some preschool age children frequently wheeze when they get colds but don’t go on to develop chronic asthma. “But some kids start wheezing at age 3, and the problem continues,” says Lemanske. “These kids also tend to be more allergic.”
A doctor will test for asthma by doing a physical exam and asking about your medical history to learn when and how often your symptoms occur. Your doctor may also ask you to breathe in and blow out into the tube of a spirometer. This device measures how much air you can breathe out and how fast you can do it.
“It’s sometimes tough to do a spirometry test on young children,” says Dr. Michelle Freemer, an NIH asthma expert. For youngsters, a doctor will do a physical exam and may perform other tests to identify possible asthma triggers.
Whether you’re young or older, it’s important to know how to manage your asthma. Work with your doctor to develop a written asthma action plan. (Here’s a sample asthma action plan from NIH). Your action plan should spell out the daily treatment plan to help control your asthma. This may include recommendations for medications and for avoiding exposure to your triggers. The action plan should also give specific instructions for what to do when asthma symptoms start and what actions to take if symptoms worsen, including when to seek medical attention, go to the hospital, or call an ambulance.
“Patients with asthma should have an action plan, so they know if they’re getting into trouble and what to do about it,” Freemer says.
For some patients, Freemer notes that a hand-held device called a peak flow meter can help you monitor your asthma. You blow into the device to measure how strongly your lungs can force air out. If the meter shows that your air flow is lower than normal, you can use your action plan to adjust your treatment.
“There are 2 main types of medicines for managing asthma: quick-relief and long-term controllers,” says Levine. Quick-relief medicines—such as short-acting bronchodilator inhalers—are used to relax the muscles in the airways to make it easier to breathe within a few minutes. If exercise is an asthma trigger, doctors may recommend taking this medicine 5 to 15 minutes before exercise or strenuous activity.
Long-term control medicines—such as inhaled corticosteroids—are used every day to help control symptoms and prevent asthma attacks. “Inhaled corticosteroids are recommended as the preferred long-term control medications for most children and adults,” says Freemer. “Taken daily, they help reduce inflammation to control the disease.”
If young children have trouble taking inhaled medications, there are masks and other devices that can help. Some kids are given a nebulizer, a portable machine that releases medicine in a mist.
A small percentage of people with asthma have a hard time controlling their symptoms even when they take their medicines regularly. Their airways become extremely inflamed and particularly sensitive to asthma triggers. They wheeze more, wake more throughout the night, and are at greater risk for breathing failure and trips to urgent care. If your asthma is severe, see a specialist to identify the most appropriate, personalized treatment.
The underlying causes of asthma are still unclear. Researchers believe asthma is caused by a combination of your genes and environmental factors. If you have allergies or a parent who has asthma, you’re at increased risk for the disease. Obesity and exposure to cigarette smoke may also raise the risk of developing asthma. NIH scientists are continuing to investigate the causes of this disease.
Researchers are also working to develop new approaches to help prevent and treat asthma. Levine’s team is studying the effects of house dust mites inside the home. While exposing mice to dust mites, the researchers identified a protein in the lung that blocked the development of asthma. With further research, the finding may eventually lead to new approaches for preventing or controlling asthma symptoms in people.
If you or your loved ones have asthma, identify your triggers and try to avoid them. Monitor your symptoms, and take prescribed medications regularly.
“For most people with asthma, if you take your prescribed medicines and stay away from the triggers, you’ll do well,” Levine says. Keep your asthma under control so you can keep living life to the fullest.
Asthma is a common, long-lasting disease that affects the lungs.
Without proper care, asthma can become serious, even deadly. But most people with asthma learn to manage the disease so they have few symptoms or none at all.
Asthma signs and symptoms include:
● Shortness of breath.
● Chest tightness or pain.
● Wheezing when exhaling, which is a common sign of asthma in children.
● Trouble sleeping caused by shortness of breath, coughing or wheezing.
● Coughing or wheezing attacks that are worsened by a respiratory virus, such as a cold or the flu. Asthma Causes and Triggers
● Infections like sinusitis, colds, and the flu.
● Allergens such as pollens, mold, pet dander, and dust mites.
● Irritants like strong odors from perfumes or cleaning solutions.
● Air pollution.
● Tobacco smoke.
● Exercise.
● Cold air or changes in the weather, such as temperature or humidity.
Take your asthma medicines as prescribed.
Asthma medicines are usually inhaled through a machine called a nebulizer, through a small device called a metered dose inhaler (also called an inhaler, puffer or MDI) or through a dry powder inhaler (DPI). For inhalers to work well, you must use them correctly. But more than half of all people who use inhalers don’t use them properly. Ask your doctor or pharmacist to watch you and check your technique. Discuss each of your asthma medications with your doctor or pharmacist.
How to use Metered Dose Inhaler (MDI)
https://youtu.be/fHYTz-ZoRLw

Nebulizers are especially good for infants' or small children's asthma medications. They can also be used for longer periods, making a potentially life-saving devices for someone suffering from a severe asthma attack.
https://www.aafa.org/asthma-prevention, NIH
Is It COVID-19, the Flu, a Cold, Allergies or Asthma? (printable PDF)
Smoking and Your Heart

Smoking tobacco can cause many health problems. Did you know that it can harm your heart and blood vessels? Smoking is a risk factor for heart disease, which can lead to heart attack, heart failure, and death. About one of every three people in the U.S. dies from heart disease.
Tobacco smoke contains many toxic chemicals. Once those chemicals get inside your body, they travel around in your blood. They can damage your heart and blood vessels. They also affect the cholesterol and fats in your blood.
All this damage can help fats and other debris build up on blood vessels. The blood vessels can become narrower. That prevents blood from flowing through as easily. Not as much oxygen and nutrients can get to the heart. That’s how heart disease develops.
Those narrow blood vessels also raise your blood pressure. That pressure puts stress on your heart.
You can reduce your risk of heart disease by not smoking. Avoiding secondhand smoke also reduces your risk
●Develop regular sleep habits; this means keeping a regular sleep and wake time, sleeping as much as needed to feel refreshed the following day, but not spending more time in bed than needed
● Avoid staying in bed in the morning to catch up on sleep
● Avoid daytime naps; if a nap is necessary, keep it short (less than 1 hour) and avoid napping after 3 pm
● Keep a regular daytime schedule; regular times for meals, medications, chores, and other activities helps keep the inner body clock running smoothly
● Do not read, write, eat, watch TV, talk on the phone, or play cards in bed
● Avoid caffeine after lunch; avoid alcohol within 6 hours of bedtime; avoid nicotine before bedtime
● Do not go to bed hungry, but do not eat a big meal near bedtime either
● Avoid sleeping pills, particularly over-the-counter remedies
● Slow down and unwind before bed (beginning at least 30 minutes before bedtime (a light snack may be helpful); create a bedtime ritual such as getting ready for bed, wearing night clothes, listening to relaxing music, or reading a magazine, newspaper, or book
● Avoid watching TV in the bedroom or sleeping on the sofa and then going to bed later in the night
● Avoid stimulating activities prior to bedtime (eg, vigorous exercise, discussing or reviewing finances, or discussing stressful issues with a spouse or partner or ruminating about them with oneself)
● Keep the bedroom dark, quiet, and at a comfortable temperature
● Exercise daily; this is best performed in the late afternoon or early evening (but not later than 6-7 pm)
● Do not force yourself to sleep; if you are unable to fall asleep within 15-30 minutes, get up and do something relaxing until sleepy (eg, read a book in a dimly lit room, watch a non-stimulating TV program); avoid watching the clock or worrying about the perceived consequences of not getting enough sleep
Desarrollar hábitos de sueño regulares; Esto significa mantener un horario regular para dormir y despertarse, dormir tanto como sea necesario para sentirse renovado al día siguiente, pero no pasar más tiempo en la cama del necesario. Evite quedarse en la cama por la mañana para recuperar el sueño. Evite las siestas durante el día; si es necesaria una siesta, hágalo breve (menos de 1 hora) y evite tomar una siesta después de las 3 pm Mantenga un horario diurno regular; horarios regulares para las comidas, medicamentos, quehaceres y otras actividades ayudan a mantener el reloj interno del cuerpo funcionando sin problemas No lea, escriba, coma, vea televisión, hable por teléfono ni juegue cartas en la cama Evite la cafeína después del almuerzo; evite el alcohol dentro de las 6 horas antes de acostarse; evitar la nicotina antes de acostarse No se vaya a la cama con hambre, pero tampoco coma una comida abundante cerca de la hora de acostarse Evite las pastillas para dormir, especialmente los remedios de venta libre Disminuya la velocidad y relájese antes de acostarse (comenzando al menos 30 minutos antes de acostarse (un refrigerio ligero puede ser útil); cree un ritual a la hora de acostarse, como prepararse para acostarse, ponerse ropa de dormir, escuchar música relajante o leer una revista, un periódico, o reservar Evite ver televisión en el dormitorio o dormir en el sofá y luego acostarse más tarde en la noche. Evite actividades estimulantes antes de acostarse (p. Ej., Ejercicio vigoroso, discutir o revisar las finanzas, discutir mas estresantes con su cónyuge o pareja o reflexionar sobre ellos con uno mismo) Mantenga el dormitorio oscuro, silencioso y a una temperatura agradable Ejercitarte diariamente; Esto se realiza mejor al final de la tarde o temprano en la noche (pero no más tarde de las 6 a las 7 pm) No se obligue a dormir; si no puede conciliar el sueño en 15-30 minutos, levántese y haga algo relajante hasta que enga sueño (por ejemplo, lea un libro en una habitación con poca luz, mire un programa de televisión que no sea estimulante); Evite mirar el reloj o preocuparse por las consecuencias percibidas de no dormir lo suficient
Prevent another UTI:
● Empty your bladder often. Urinate and empty your bladder as soon as you feel the need. Do not hold your urine for long periods of time.
● Wipe from front to back after you urinate or have a bowel movement. This will help prevent germs from getting into your urinary tract through your urethra.
● Drink liquids as directed. Ask how much liquid to drink each day and which liquids are best for you. You may need to drink more liquids than usual to help flush out the bacteria. Do not drink alcohol, caffeine, or citrus juices. These can irritate your bladder and increase your symptoms. Your healthcare provider may recommend cranberry juice to help prevent a UTI.
● Urinate after you have sex. This can help flush out bacteria passed during sex.
● Do not douche or use feminine deodorants. These can change the chemical balance in your vagina.
● Change sanitary pads or tampons often. This will help prevent germs from getting into your urinary tract.
● Do pelvic muscle exercises often. Pelvic muscle exercises may help you start and stop urinating. Strong pelvic muscles may help you empty your bladder easier. Squeeze these muscles tightly for 5 seconds like you are trying to hold back urine. Then relax for 5 seconds. Gradually work up to squeezing for 10 seconds. Do 3 sets of 15 repetitions a
Prevenir otra ITU: Vacíe su vejiga a menudo. Orine y vacíe su vejiga tan pronto como sienta la necesidad. No retenga la orina durante largos períodos de tiempo. Limpie de adelante hacia atrás después de orinar o evacuar. Esto ayudará a evitar que los gérmenes entren a su tracto urinario a través de la uretra. Beba líquidos según las indicaciones. Pregunte cuánto líquido debe beber cada día y qué líquidos son mejores para usted. Es posible que deba beber más líquidos de lo habitual para ayudar a eliminar la bacteria. No tome alcohol, cafeína o jugos cítricos. Estos pueden irritar su vejiga y aumentar sus síntomas. Su proveedor de atención médica puede recomendar el jugo de arándano para ayudar a prevenir una ITU. Orina después de tener relaciones sexuales. Esto puede ayudar a eliminar las bacterias que pasan durante el sexo. No se douche o use desodorantes femeninos. Estos pueden cambiar el equilibrio químico en su vagina. Cambie las toallas sanitarias o los tampones a menudo. Esto ayudará a evitar que los gérmenes entren a su tracto urinario. Haga ejercicios musculares pélvicos a menudo. Los ejercicios de los músculos pélvicos pueden ayudarlo a comenzar y dejar de orinar. Los músculos pélvicos fuertes pueden ayudarlo a vaciar su vejiga más fácilmente. Aprieta estos músculos con fuerza durante 5 segundos como si estuvieras intentando retener la orina. Luego relájate durante 5 segundos. Poco a poco trabajar hasta apretar durante 10 segundos. Haga 3 series de 15 repeticiones al día, o según las indicaciones
Stop TB
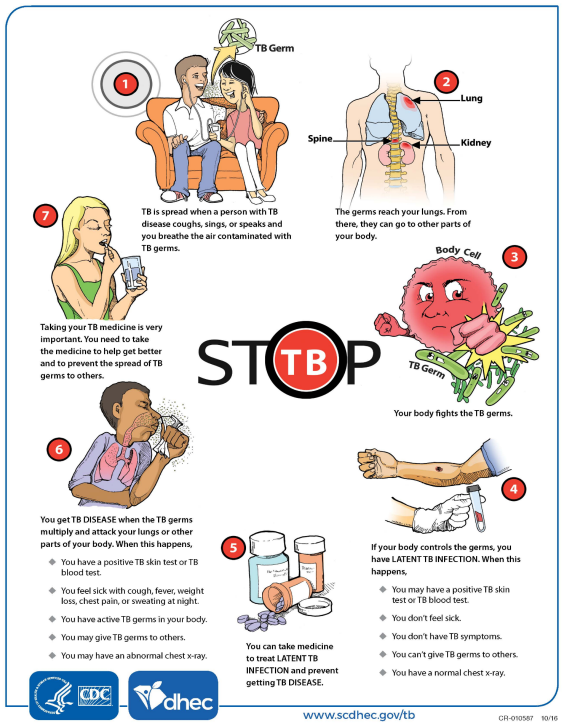
Some signs of TB disease are: • A bad cough that lasts 3 weeks or longer. • Pain in the chest. • Coughing up blood or phlegm from deep inside the lungs. • Weakness or feeling very tired. • Losing weight without trying. • Having no appetite. • Chills and fever. • Sweating at night or when you are sleeping
TB germs can sometimes stay alive in the air for a few hours, especially in small places with no fresh air. Fresh air and sunlight make it harder for TB germs to stay alive. The fresh air scatters the germs and the sunlight kills them
You will probably start off with several TB medicines. • You will need to take your medicines the right way, just as your doctor or healthcare provider tells you. • You will need to stay on TB medicines for at least 6 months.
Take isoniazid on an empty stomach, at least 1 hour before or 2 hours after a meal. Use this medicine for the full prescribed length of time. Your symptoms may improve before the infection is completely cleared. Skipping doses may also increase your risk of further infection that is resistant to antibiotics.
Take INH at night before bedtime (1 hour before or 2 hours after eating). 9 If the medication upsets your stomach, you may take it with a snack. 9 If you have diabetes, your blood sugars may change. DO NOT: 9 consume alcohol while taking INH. 9 use Tylenol (acetaminophen) or any medications containing this drug while you are on INH. AVOID: 9 taking aluminum-based antacids (Maalox or Mylanta, for example).
Algunos signos de la enfermedad de la tuberculosis son: • Una tos fuerte que dura 3 semanas o más. • Dolor en el pecho. • Toser sangre o flema desde el interior de los pulmones. • Debilidad o sentirse muy cansado. • Bajar de peso sin intentarlo. • Falta de apetito. • Escalofríos y fiebre. • Sudar por la noche o cuando duerme.
Los gérmenes de la tuberculosis a veces pueden permanecer vivos en el aire durante algunas horas, especialmente en lugares pequeños sin aire fresco. El aire fresco y la luz solar dificultan la vida de los gérmenes de la tuberculosis. El aire fresco esparce los gérmenes y la luz del sol los mata.
Probablemente comenzará con varios medicamentos para la tuberculosis. • Deberá tomar sus medicamentos de la manera correcta, tal como le indique su médico o proveedor de atención médica. • Deberá seguir tomando los medicamentos para la tuberculosis durante al menos 6 meses. Tome isoniazid con el estómago vacío, al menos 1 hora antes o 2 horas después de una comida. Use este medicamento durante todo el tiempo prescrito. Sus síntomas pueden mejorar antes de que la infección desaparezca por completo. Omitir dosis también puede aumentar el riesgo de una mayor infección que sea resistente a los antibióticos.
Tome INH por la noche antes de acostarse (1 hora antes o 2 horas después de comer). 9 Si el medicamento le produce malestar estomacal, puede tomarlo con un refrigerio. 9 Si tiene diabetes, sus niveles de azúcar en sangre pueden cambiar. NO DEBE: 9 consumir alcohol mientras toma INH. 9 use Tylenol (acetaminofén) o cualquier medicamento que contenga este
Keep your nails short to limit any damage done to your skin by scratching. As much as possible try not to scratch. It is thought that scratching can make itch worse and you may get into an 'itch-scratch' vicious cycle. (That is, you itch more because you scratch, so you scratch more because you itch more ... and so on.)
Keep cool as much as possible. Some people find having cool (or lukewarm) baths or showers soothing. Avoid irritants such as soaps, bubble bath and detergents. Cotton clothes are usually preferable to woollen clothes.
Moisturisers (emollients). Dry skin may be making the itch worse. Moisturisers are useful to keep the skin supple and moist. They can be applied once a day or several times a day if your skin becomes very dry. Water and soap dry out the skin as they wash away the natural skin oils. Therefore, the most important time to use moisturisers is after a bath or shower. Moisturisers work by providing a replacement for these body oils and keeping the skin moist. Numerous moisturisers are available as creams, ointments and bath/shower additives, and also to use instead of soap. It may be worth trying out a few to see which is the most suitable. These can be bought over-the-counter or different ones are available on prescription from your doctor. Use them liberally, as often as needed.
Mantenga sus uñas cortas para limitar cualquier daño causado a su piel al rascarse. En la medida de lo posible, trate de no rayar. Se cree que rascarse puede empeorar la picazón y puede entrar en un círculo vicioso de "picazón-rascado". (Es decir, te pica más porque te rascas, entonces te rascas más porque te pica más ... y así sucesivamente). Manténgase fresco tanto como sea posible. Algunas personas encuentran reconfortante tomar baños o duchas fríos (o tibios). Evite irritantes como jabones, baños de burbujas y detergentes. La ropa de algodón suele ser preferible a la ropa de lana. Hidratantes (emolientes). La piel seca puede empeorar la picazón. Los humectantes son útiles para mantener la piel tersa y húmeda. Se pueden aplicar una vez al día o varias veces al día si tu piel se vuelve muy seca. El agua y el jabón secan la piel mientras eliminan los aceites naturales de la piel. Por lo tanto, el momento más importante para usar humectantes es después del baño o la ducha. Los humectantes actúan reemplazando estos aceites corporales y manteniendo la piel húmeda. Numerosos humectantes están disponibles como cremas, ungüentos y aditivos para el baño / ducha, y también para usar en lugar de jabón. Puede valer la pena probar algunos para ver cuál es el más adecuado. Estos se pueden comprar sin receta o hay diferentes disponibles con receta de su médico. Úselos generosamente, tantas veces como sea necesario.Moisturisers (emollients): These should be applied several times every day to help the outer layer of skin to function better as a barrier to the environment. The drier the skin, the more frequently moisturiser should be applied. Many different moisturisers are available, varying in their degree of greasiness, and it is important to choose the most suitable to use Topical steroid creams or ointments: Apply twice daily. These will usually improve the redness and itching. Avoidance of Allergens: Atopic people often have allergies: Air borne allergens from cats, dogs, pollen, grass or the house dustmite, can cause flare-ups of atopic eczema for some patients. Latex (rubber) allergy is more common in people who have atopic eczema. The symptoms may, consist only of itching of the skin after contact with rubber products. Contact allergy to creams and ointments used to treat atopic eczema can rarely occur. It is advisable to inform the doctor know if treatments seem to be making the skin worse (see Patient Information Leaflet on Contact Dermatitis)
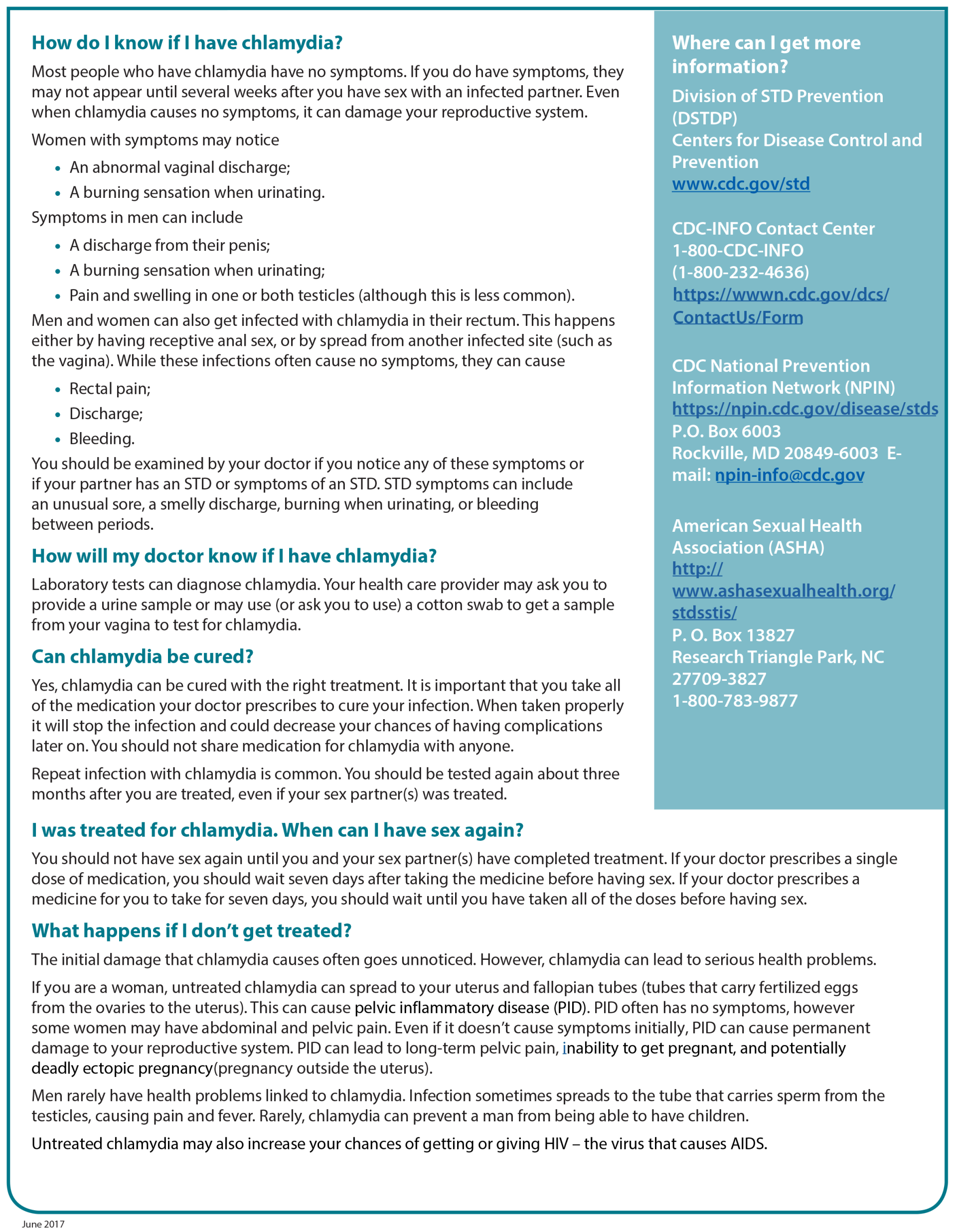
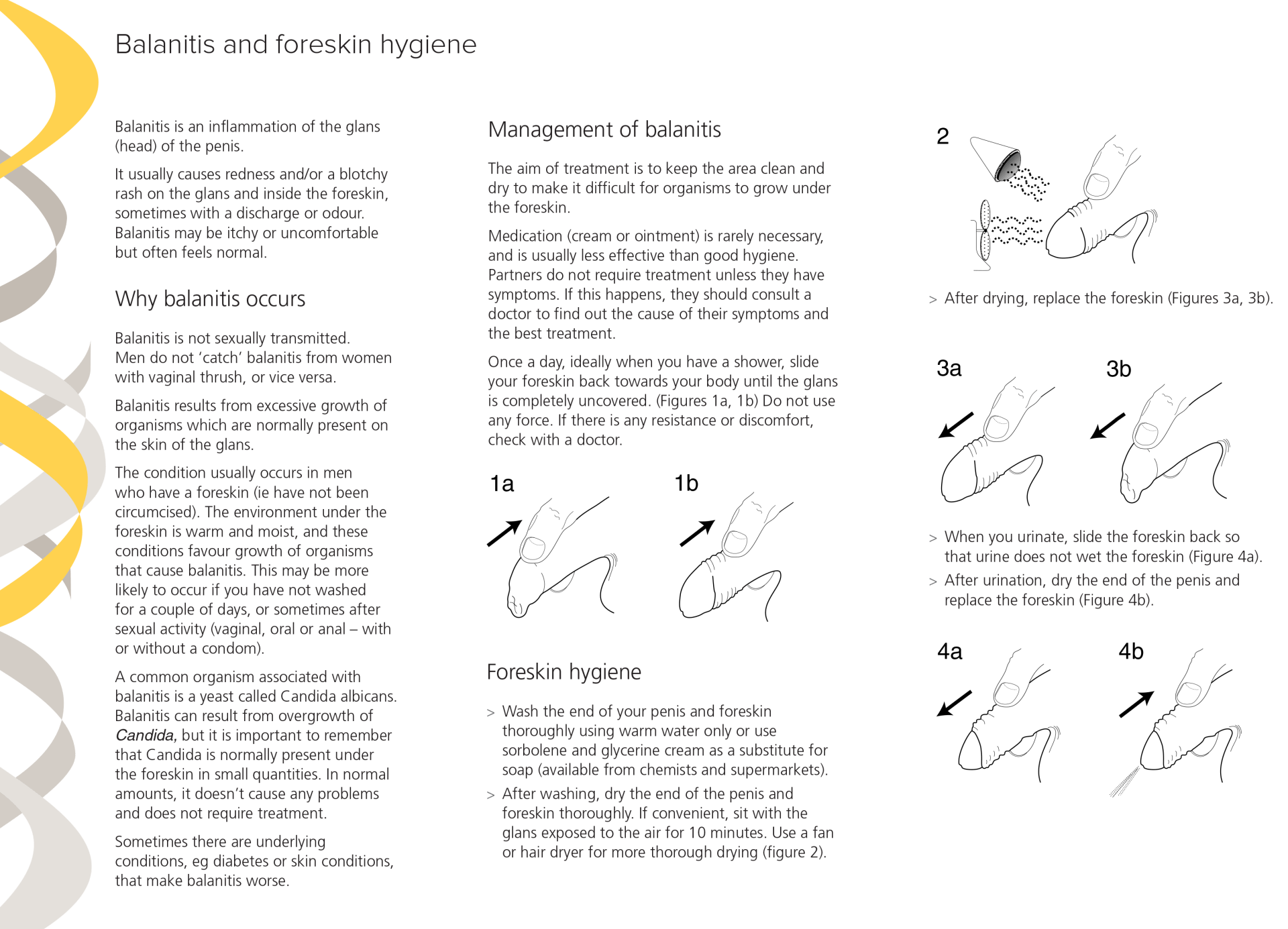
Balanitis e higiene del prepucio
Si es propenso a desarrollar balanitis unas horas después de tener relaciones sexuales, lave el pene como se describe poco después de tener relaciones sexuales. Asegúrese de que el glande esté completamente seco antes de reemplazar el prepucio. Estas medidas deberían conducir a una rápida mejora de los síntomas y ayudar a prevenir la balanitis en el futuro. Balanitis recurrente Debido a que Candida y otros organismos normalmente están presentes debajo del prepucio, es posible que los hombres experimenten más episodios de balanitis. No existe un tratamiento para "curar" permanentemente la balanitis o erradicar los organismos que la causan. Si experimenta ataques repetidos de balanitis a pesar de una higiene adecuada del prepucio, consulte a su médico.
e es difícil para los organismos crecer debajo del prepucio. Rara vez se necesita medicación (crema o ungüento) y, por lo general, es menos eficaz que una buena higiene. Las parejas no necesitan tratamiento a menos que presenten síntomas. Si esto sucede, deben consultar a un médico para averiguar la causa de sus síntomas y el mejor tratamiento. Una vez al día, idealmente cuando te duches, desliza el prepucio hacia tu cuerpo hasta que el glande esté completamente descubierto. (Figuras 1a, 1b) No aplique fuerza. Si hay alguna resistencia o malestar, consulte con un médico. La balanitis es una inflamación del glande (cabeza) del pene. Por lo general, causa enrojecimiento y / o una erupción con manchas en el glande y dentro del prepucio, a veces con secreción u olor. La balanitis puede causar picazón o ser incómoda, pero a menudo se siente normal. Por qué ocurre la balanitis La balanitis no se transmite sexualmente. Los hombres no "contraen" balanitis de mujeres con candidiasis vaginal, o viceversa. La balanitis es el resultado del crecimiento excesivo de organismos que normalmente están presentes en la piel del glande. La afección generalmente ocurre en hombres que tienen prepucio (es decir, que no han sido circuncidados). El ambiente debajo del prepucio es cálido y húmedo, y estas condiciones favorecen el crecimiento de organismos que causan balanitis. Es más probable que esto ocurra si no se ha lavado durante un par de días o, a veces, después de la actividad sexual (vaginal, oral o anal, con o sin condón). Un organismo común asociado con la balanitis es una levadura llamada Candida albicans. La balanitis puede resultar de un crecimiento excesivo de Candida, pero es importante recordar que Candida normalmente está presente debajo del prepucio en pequeñas cantidades. En cantidades normales, no causa ningún problema y no requiere tratamiento. A veces hay afecciones subyacentes, por ejemplo, diabetes o afecciones de la piel, t Manejo de la balanitis El objetivo del tratamiento es mantener el área limpia y seca para dificultar el crecimiento de organismos debajo del prepucio. Rara vez se necesita medicación (crema o ungüento) y, por lo general, es menos eficaz que una buena higiene. Las parejas no necesitan tratamiento a menos que presenten síntomas. Si esto sucede, deben consultar a un médico para averiguar la causa de sus síntomas y el mejor tratamiento. Una vez al día, idealmente cuando te duches, desliza el prepucio hacia tu cuerpo hasta que el glande esté completamente descubierto. (Figuras 1a, 1b) No aplique fuerza. Si hay alguna resistencia o malestar, consulte con un médico. La balanitis es una inflamación del glande (cabeza) del pene. Por lo general, causa enrojecimiento y / o una erupción con manchas en el glande y dentro del prepucio, a veces con secreción u olor. La balanitis puede causar picazón o ser incómoda, pero a menudo se siente normal. Por qué ocurre la balanitis La balanitis no se transmite sexualmente. Los hombres no "contraen" balanitis de mujeres con candidiasis vaginal, o viceversa. La balanitis es el resultado del crecimiento excesivo de organismos que normalmente están presentes en la piel del glande. La afección generalmente ocurre en hombres que tienen prepucio (es decir, que no han sido circuncidados). El ambiente debajo del prepucio es cálido y húmedo, y estas condiciones favorecen el crecimiento de organismos que causan balanitis. Es más probable que esto ocurra si no se ha lavado durante un par de días o, a veces, después de la actividad sexual (vaginal, oral o anal, con o sin condón). Un organismo común asociado con la balanitis es una levadura llamada Candida albicans. La balanitis puede resultar de un crecimiento excesivo de Candida, pero es importante recordar que Candida normalmente está presente debajo del prepucio en pequeñas cantidades. En cantidades normales, no causa ningún problema y no requiere tratamiento. A veces, hay afecciones subyacentes, por ejemplo, diabetes o afecciones de la piel, que empeoran la balanitis. Balanitis e higiene del prepucio Higiene del prepucio> Lave bien la punta del pene y el prepucio con agua tibia solamente o use crema de sorboleno y glicerina como sustituto del jabón (disponible en farmacias y supermercados). > Después del lavado, seque bien la punta del pene y el prepucio. Si es conveniente, siéntese con el glande expuesto al aire durante 10 minutos. Use un ventilador o secador de pelo para un secado más completo (figura 2).
Bacterial Vaginosis
Bacteriana La Vaginosis bacteriana (VB) es una infección en la vagina. La VB es causada por cambios en la cantidad de ciertos tipos de bacterias en su vagina. La VB es la infección vaginal más común en mujeres de 15 a 44 años. La VB se puede tratar fácilmente con medicamentos de su médico o enfermera. Si no se trata, puede aumentar el riesgo de contraer infecciones de transmisión sexual (ITS), como el VIH, el herpes genital, la clamidia y la gonorrea.
Puede contraer VB sin tener relaciones sexuales, pero la VB también puede ser causada por relaciones sexuales vaginales, orales o anales. Puede contraer VB de parejas masculinas o femeninas. Puede tener un mayor riesgo de contraer VB si: Tiene una nueva pareja sexual Tiene varias parejas sexuales Ducha No usa condones Está embarazada
Muchas mujeres no presentan signos ni síntomas.
Si tiene síntomas, estos pueden incluir:
- Flujo vaginal inusual. La secreción puede ser blanca (lechosa) o gris. También puede ser espumoso o acuoso. Algunas mujeres informan de un fuerte olor a pescado, especialmente después de las relaciones sexuales.
- Ardor al orinar
- Picazón alrededor del exterior de la vagina
- Irritación vaginal Estos síntomas pueden ser similares a las infecciones vaginales por hongos y otros problemas de salud.
Bacterial Vaginosis Bacterial vaginosis (BV) is an infection in the vagina. BV is caused by changes in the amount of certain types of bacteria in your vagina. BV is the most common vaginal infection in women ages 15 to 44. BV is easily treatable with medicine from your doctor or nurse. If left untreated, it can raise your risk for sexually transmitted infections (STIs), including HIV, genital herpes, chlamydia, and gonorrhea.. . You can get BV without having sex, but BV can also be caused by vaginal, oral, or anal sex. You can get BV from male or female partners. You may be more at risk for BV if you: Have a new sex partner Have multiple sex partners Douche Do not use condoms Are pregnant.
Many women have no signs or symptoms.
If you do have symptoms, they may include:
- Unusual vaginal discharge. The discharge can be white (milky) or gray. It may also be foamy or watery. Some women report a strong fish-like odor, especially after sex.
- Burning when urinating
- Itching around the outside of the vagina
- Vaginal irritation These symptoms may be similar to vaginal yeast infections and other health problems.
See a doctor or nurse. Antibiotics will treat BV. Take all of your medicine. Even if symptoms go away, you need to finish all of the antibiotic. Avoid sexual contact until you finish your treatment. S teps you can take to lower your risk of BV include: Help keep your vaginal bacteria balanced. Use only warm water to clean the outside of your vagina. You do not need to use soap. Bacterial Vaginosis 2 Even mild soap can cause infection or irritate your vagina. Always wipe front to back from your vagina to your anus. Do not douche. Douching removes some of the normal bacteria in your vagina that protect you from infection. Doctors do not recommend douching. Practice safe sex. The best way to prevent the spread of BV through sex is by not having sex. If you do have sex, you can lower your risk of getting BV, or any STI, with the following steps: Use condoms. Condoms are the best way to prevent BV or STIs when you have sex. Make sure to put on the condom before the penis touches your vagina, mouth, or anus. Other methods of birth control, like birth control pills, shots, implants, or diaphragms, will not protect you from STIs. Get tested. Be sure you and your partner are tested for STIs. Talk to each other about your test results before you have sex. Be monogamous. Having sex with just one partner can lower your risk. Be faithful to each other. That means that you only have sex with each other and no one else. Limit your number of sex partners. Your risk of getting BV and STIs goes up with the number of partners you have. Don’t abuse alcohol or drugs, which are linked to sexual risk taking. Drinking too much alcohol or using drugs also puts you at risk of sexual assault and possible exposure to STIs.
YEAST INFECTION
How can I keep from getting another infection?
Here are some things you can do to help prevent another yeast infection:
- Do not wear tight-fitting or synthetic-fiber clothes.
- Wear cotton underwear.
- Wipe from front to back after using the toilet. This may help keep the bacteria that normally live in your rectum from getting into your vagina.
- Do not douche or use feminine hygiene sprays.
- Avoid deodorant sanitary pads or tampons, or bubble bath, and avoid using colored or perfumed toilet paper.
- If you get many yeast infections, your doctor may recommend you use medicines regularly for a few months to prevent more yeast infections.
bacteriana La vaginosis bacteriana (VB) es una infección en la vagina. La VB es causada por cambios en la cantidad de ciertos tipos de bacterias en su vagina. La VB es la infección vaginal más común en mujeres de 15 a 44 años. La VB se puede tratar fácilmente con medicamentos de su médico o enfermera. Si no se trata, puede aumentar el riesgo de contraer infecciones de transmisión sexual (ITS), como el VIH, el herpes genital, la clamidia y la gonorrea. . Puede contraer VB sin tener relaciones sexuales, pero la VB también puede ser causada por relaciones sexuales vaginales, orales o anales. Puede contraer VB de parejas masculinas o femeninas. Puede tener un mayor riesgo de contraer VB si: Tiene una nueva pareja sexual Tiene varias parejas sexuales Ducha No usa condones Está embarazada. Muchas mujeres no presentan signos ni síntomas.
Si tiene síntomas, estos pueden incluir:
- Flujo vaginal inusual. La secreción puede ser blanca (lechosa) o gris. También puede ser espumoso o acuoso. Algunas mujeres informan de un fuerte olor a pescado, especialmente después de las relaciones sexuales.
- Ardor al orinar
- Picazón alrededor del exterior de la vagina
- Irritación vaginal Estos síntomas pueden ser similares a las infecciones vaginales por hongos y otros problemas de salud.
Consulte a un médico o enfermero. Los antibióticos tratarán la VB. Tome todos sus medicamentos. Incluso si los síntomas desaparecen, debe terminar todo el antibiótico. Evite el contacto sexual hasta que termine su tratamiento. Las medidas que puede tomar para reducir el riesgo de VB incluyen: Ayudar a mantener el equilibrio de las bacterias vaginales. Use solo agua tibia para limpiar el exterior de su vagina. No es necesario utilizar jabón. Vaginosis bacteriana 2 Incluso un jabón suave puede provocar una infección o irritar la vagina. Siempre límpiese de adelante hacia atrás desde la vagina hasta el ano. No te duches. Las duchas vaginales eliminan algunas de las bacterias normales de la vagina que la protegen de las infecciones. Los médicos no recomiendan las duchas vaginales. Practica sexo seguro. La mejor manera de prevenir la propagación de la VB a través del sexo es no tener relaciones sexuales. Si tiene relaciones sexuales, puede reducir el riesgo de contraer VB o cualquier ITS siguiendo estos pasos: Use condones. Los condones son la mejor manera de prevenir la VB o las ITS cuando tiene relaciones sexuales. Asegúrese de ponerse el condón antes de que el pene toque su vagina, boca o ano. Otros métodos anticonceptivos, como píldoras anticonceptivas, inyecciones, implantes o diafragmas, no la protegerán de las ITS. Hacerse la prueba. Asegúrese de que usted y su pareja se hagan la prueba de detección de ITS. Hablen sobre los resultados de sus pruebas antes de tener relaciones sexuales. Sea monógamo. Tener relaciones sexuales con una sola pareja puede reducir su riesgo. Sed fieles el uno al otro. Eso significa que solo tienen relaciones sexuales entre ustedes y con nadie más. Limite su número de parejas sexuales. Su riesgo de contraer VB e ITS aumenta con la cantidad de parejas que tenga. No abuse del alcohol o las drogas, que están relacionadas con la asunción de riesgos sexuales. Beber demasiado alcohol o consumir drogas también lo pone en riesgo de sufrir agresión sexual y una posible exposición a las ITS.
Ear Pain
How can I avoid getting ear infections/pain?
Avoid getting water, soap or shampoo into the ear canal when having a bath or shower. Place a piece of cotton wool at the entrance of both ear canals. Do not push the cotton wool down into the ear canal as it may be difficult to remove. To clean the outside of the ear use a dry tissue, or alcohol-free baby wipes, around and behind the ear after showering or bathing. Make sure you never use cotton buds, tissues or material to soak up any moisture in your ears. Let them dry naturally. Do not use cotton buds, scratch or poke your ears, or insert anything into your ears. To keep your ears dry when swimming you may consider wearing a tight-fitting swimming cap over your ears. Headbands are also available to protect the ears from water. This will also help to keep cotton wool or earplugs in place. If you suffer from frequent bouts of otitis externa it may be helpful to visit your doctor This service may be provided for you by the NHS. Ask your GP or practice nurse to refer you. If you accidentally get water in your ears, speak to your doctor about treatments to reduce the chance of a recurring infection. If you suffer from itchy or dry skin in your ear canals speak to your doctoror a healthcare professional about treatments available. If the entrance to the ear canal is dry and/or itchy, you may find it helpful to place a moisturising ointment around the bowl of the ear and at the entrance to the ear canal. If the otitis externa does not settle after treatment, your ear should be checked by a doctor
What happens if I do not get treatment?
The ear infection may get worse and become very painful. It will become uncomfortable to move your jaw and further complications may develop (such as the infection spreading beyond your external ear). Compress A warm compress may help relieve the pressure building up in the ear as well. Using a compress for 20-minute periods while resting can help reduce pain. ¿Cómo puedo evitar contraer infecciones / dolor de oído?
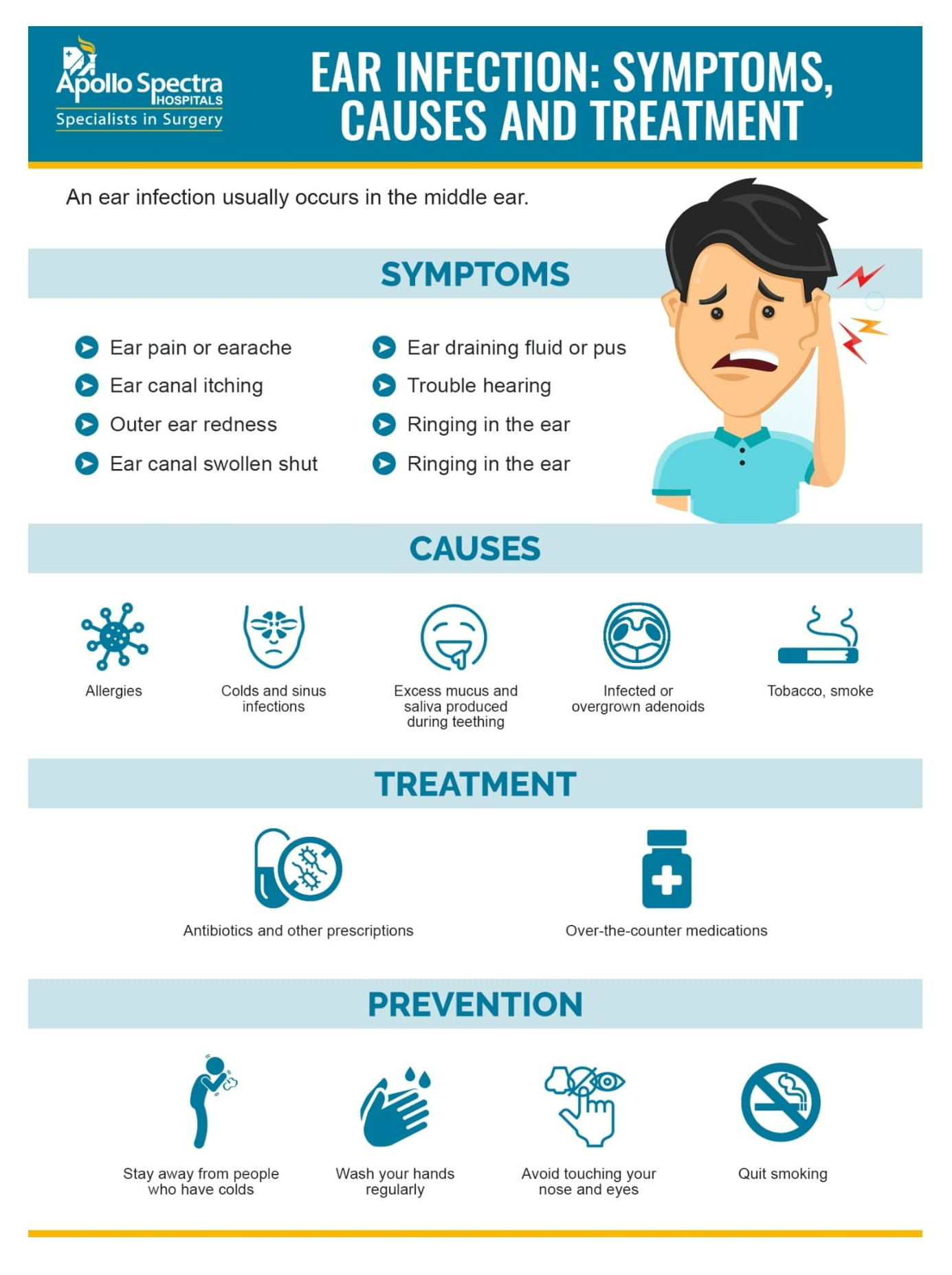
Evite que entre agua, jabón o champú en el canal auditivo cuando se bañe o se duche. Coloque un trozo de algodón en la entrada de ambos canales auditivos. No introduzca el algodón en el canal auditivo, ya que puede ser difícil de extraer. Para limpiar la parte externa de la oreja, use un pañuelo de papel seco o toallitas húmedas para bebés sin alcohol alrededor y detrás de la oreja después de ducharse o bañarse. Asegúrese de nunca utilizar bastoncillos de algodón, pañuelos de papel o material para absorber la humedad de los oídos. Déjalos secar naturalmente. No use bastoncillos de algodón, no se rasque ni se pinche las orejas, ni se meta nada en las orejas. Para mantener sus oídos secos al nadar, puede considerar usar un gorro de natación ajustado sobre sus oídos. También hay disponibles diademas para proteger los oídos del agua. Esto también ayudará a mantener el algodón o los tapones para los oídos en su lugar. Si sufre de episodios frecuentes de otitis externa, puede ser útil que visite a su médico. Este servicio puede ser proporcionado por el NHS. Pídale a su médico de cabecera o enfermera de práctica que lo derive. Si accidentalmente le entra agua en los oídos, hable con su médico sobre los tratamientos para reducir la posibilidad de una infección recurrente. Si sufre de picazón o sequedad en la piel en los canales auditivos, hable con su médico o un profesional de la salud sobre los tratamientos disponibles. Si la entrada al canal auditivo está seca y / o le pica, puede resultarle útil colocar una pomada humectante alrededor del cuenco del oído y en la entrada del canal auditivo. Si la otitis externa no desaparece después del tratamiento, un médico debe examinarle el oído. ¿Qué pasa si no recibo tratamiento? La infección del oído puede empeorar y volverse muy dolorosa. Le resultará incómodo mover la mandíbula y se pueden desarrollar más complicaciones (como la propagación de la infección más allá del oído externo). Comprimir Una compresa tibia también puede ayudar a aliviar la presión acumulada en el oído. Usar una compresa durante períodos de 20 minutos en reposo puede ayudar a reducir el dolor.
Superbugs
Help Fight Drug-Resistant Bacteria
For nearly a century, bacteria-fighting drugs known as antibiotics have helped to control and destroy many of the harmful bacteria that can make us sick. But in recent decades, antibiotics have been losing their punch against some types of bacteria. In fact, certain bacteria are now unbeatable with today’s medicines. Sadly, the way we’ve been using antibiotics is helping to create new drug-resistant “superbugs.”
Superbugs are strains of bacteria that are resistant to several types of antibiotics. Each year these drug-resistant bacteria infect more than 2 million people nationwide and kill at least 23,000, according to the U.S. Centers for Disease Control and Prevention (CDC). Drug-resistant forms of tuberculosis, gonorrhea, and staph infections are just a few of the dangers we now face.
Antibiotics are among the most commonly prescribed drugs for people. They’re also given to livestock to prevent disease and promote growth. Antibiotics are effective against bacterial infections, such as strep throat and some types of pneumonia, diarrheal diseases, and ear infections. But these drugs don’t work at all against viruses, such as those that cause colds or flu.
Unfortunately, many antibiotics prescribed to people and to animals are unnecessary. And the overuse and misuse of antibiotics helps to create drug-resistant bacteria.
Here’s how that might happen. When used properly, antibiotics can help destroy disease-causing bacteria. But if you take an antibiotic when you have a viral infection like the flu, the drug won’t affect the viruses making you sick. Instead, it’ll destroy a wide variety of bacteria in your body, including some of the “good” bacteria that help you digest food, fight infection, and stay healthy. Bacteria that are tough enough to survive the drug will have a chance to grow and quickly multiply. These drug-resistant strains may even spread to other people.
Over time, if more and more people take antibiotics when not necessary, drug-resistant bacteria can continue to thrive and spread. They may even share their drug-resistant traits with other bacteria. Drugs may become less effective or not work at all against certain disease-causing bacteria.
“Bacterial infections that were treatable for decades are no longer responding to antibiotics, even the newer ones,” says Dr. Dennis Dixon, an NIH expert in bacterial and fungal diseases. Scientists have been trying to keep ahead of newly emerging drug-resistant bacteria by developing new drugs, but it’s a tough task.
“We need to make the best use of the drugs we have, as there aren’t many in the antibiotic development pipeline,” says Dr. Jane Knisely, who oversees studies of drug-resistant bacteria at NIH. “It’s important to understand the best way to use these drugs to increase their effectiveness and decrease the chances of resistance to emerge.”
You can help slow the spread of drug-resistant bacteria by taking antibiotics properly and only when needed. Don’t insist on an antibiotic if your health care provider advises otherwise. For example, many parents expect doctors to prescribe antibiotics for a child’s ear infection. But experts recommend delaying for a time in certain situations, as many ear infections get better without antibiotics.
NIH researchers have been looking at whether antibiotics are effective for treating certain conditions in the first place. One recent study showed that antibiotics may be less effective than previously thought for treating a common type of sinus infection. This kind of research can help prevent the misuse and overuse of antibiotics.
“Treating infections with antibiotics is something we want to preserve for generations to come, so we shouldn’t misuse them,” says Dr. Julie Segre, a senior investigator at NIH.
In the past, some of the most dangerous superbugs have been confined to health care settings. That’s because people who are sick or in a weakened state are more susceptible to picking up infections. But superbug infections aren’t limited to hospitals. Some strains are out in the community and anyone, even healthy people, can become infected.
One common superbug increasingly seen outside hospitals is methicillin-resistant Staphylococcus aureus (MRSA). These bacteria don’t respond to methicillin and related antibiotics. MRSA can cause skin infections and, in more serious cases, pneumonia or bloodstream infections.
A MRSA skin infection can appear as one or more pimples or boils that are swollen, painful, or hot to the touch. The infection can spread through even a tiny cut or scrape that comes into contact with these bacteria. Many people recover from MRSA infections, but some cases can be life-threatening. The CDC estimates that more than 80,000 aggressive MRSA infections and 11,000 related deaths occur each year in the United States.
When antibiotics are needed, doctors usually prescribe a mild one before trying something more aggressive like vancomycin. Such newer antibiotics can be more toxic and more expensive than older ones. Eventually, bacteria will develop resistance to even the new drugs. In recent years, some superbugs, such as vancomycin-resistant Enterococci bacteria, remain unaffected by even this antibiotic of last resort.
“We rely on antibiotics to deliver modern health care,” Segre says. But with the rise of drug-resistant bacteria, “we’re running out of new antibiotics to treat bacterial infections,” and some of the more potent ones aren’t working as well.
Ideally, doctors would be able to quickly identify the right antibiotic to treat a particular infection. But labs need days or even weeks to test and identify the bacteria strain. Until the lab results come in, antibiotic treatment is often an

“We need to know how to treat for a favorable outcome, but knowledge about the infection can be several days away,” explains Dr. Vance Fowler, an infectious disease expert at Duke University School of Medicine.
Fowler says faster diagnostic testing offers one of the best hopes for treating infectious diseases. Technology is catching up, he says, and new research in this area looks promising.
Genetic studies by NIH-supported researchers such as Segre and Fowler are also helping us understand the unique characteristics of antibiotic-resistant bacteria. Their findings could point the way to innovative new treatments.
While scientists search for ways to beat back these stubborn bacteria, you can help by preventing the spread of germs so we depend less on antibiotics in the first place.
The best way to prevent bacterial infections is by washing your hands frequently with soap and water. It’s also a good idea not to share personal items such as towels or razors. And use antibiotics only as directed. We can all do our part to fight drug-resistant bacteria.
Burn Care

Burns are skin or tissue damage, usually caused by heat. Burns often happen in the home. Some are caused by fire. They can also be caused by hot liquid, steam, and certain chemicals.
Burns are defined by how deep they are and how large an area they cover. First degree burns are the least serious. They affect only the thin top layer of skin. A sunburn is a common example. They usually heal on their own within a week. Second-degree burns damage the layer of skin below the outer layer as well. They may leave a scar. Third-degree burns damage or destroy the entire thickness of the skin. They require skin grafts—natural or artificial skin to cover and protect the body while it heals.
It’s important to seek medical care quickly for deep or large burns. Serious burns require professional medical care. Some can even be life-threatening. But research advances over the past few decades have increased the chances of survival for people with severe burns.
Minor burns can often be treated at home. First, clean the area with cool water and dry. Then cover with sterile gauze or a non-adhesive bandage. Avoid breaking blisters because this can cause infection. Call your doctor if the burn has not healed after several weeks or shows signs of infection. These include increased pain, swelling, and redness.
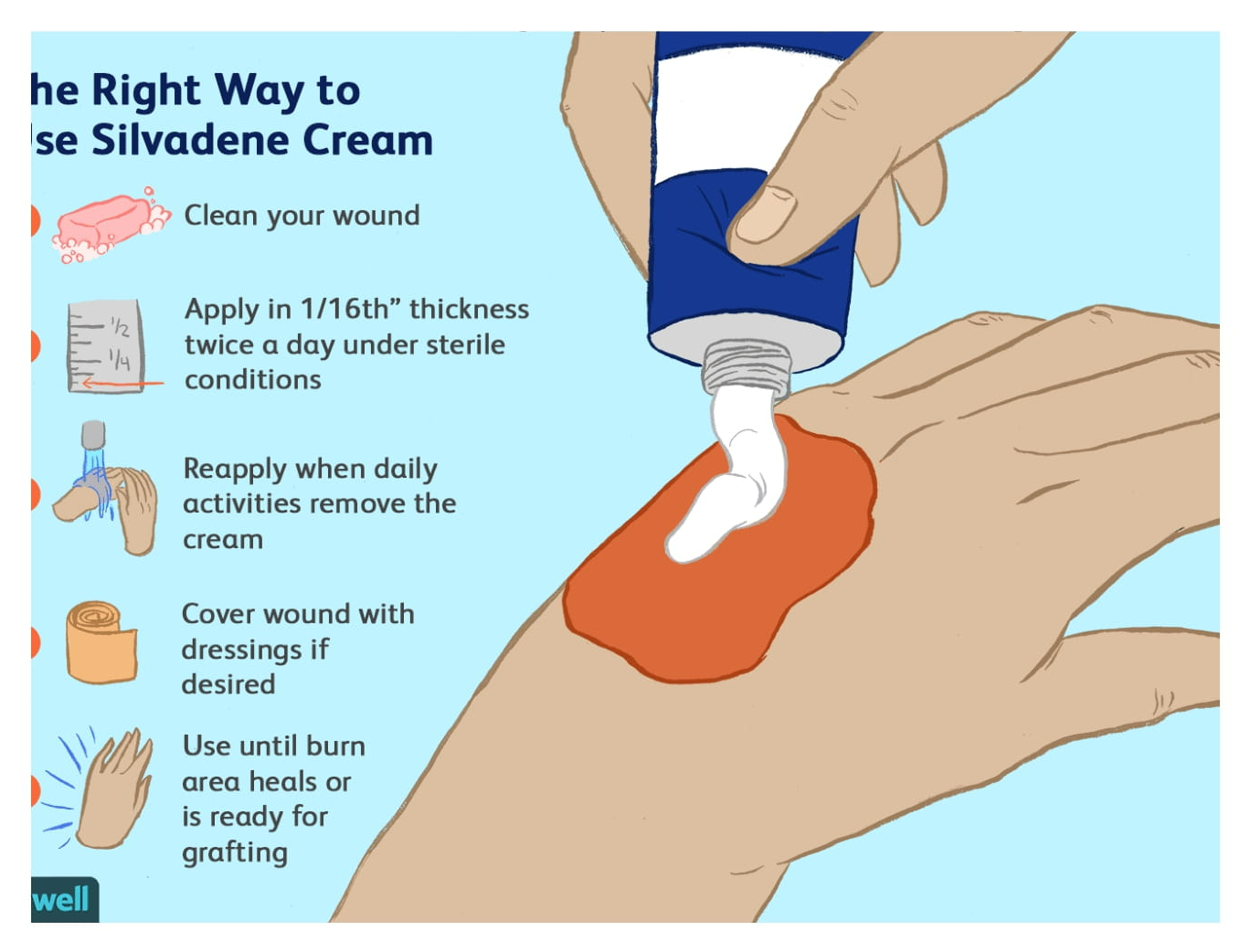
Preventing Gum Disease

The problem begins with bacteria. Our mouths are packed with these tiny microbes. They combine with mucus and other particles to form a sticky, colorless film—called plaque—on our teeth. Brushing and flossing can get rid of some plaque. But any that remains can harden and form tartar, a yellowish deposit that can become rock-hard.
Plaque and tartar buildup can lead to gum disease—technically known as periodontal disease. The most common and mild type of gum disease is called gingivitis. The gums become red and swollen, and they can bleed easily. Daily brushing and flossing and regular cleanings by dental professionals can usually clear up gingivitis.
If gingivitis is not treated, it can become a more severe type of gum disease called periodontitis. Symptoms of periodontitis include bad breath that won’t go away; gums that are red, swollen, tender or bleeding; painful chewing; and loose or sensitive teeth.
In periodontitis, the gums pull away from the teeth and form “pockets” that become infected. Bacterial toxins and your body’s natural response to infection start to break down the bone and soft tissues that hold teeth in place. If not treated, the tissues will be destroyed. Your teeth may eventually become loose and have to be removed. If you have periodontitis, your dentist may recommend a deep-cleaning method called scaling and root planing. In more severe cases, you may need surgery.
Most people don’t show signs of gum disease until they’re in their 30s or 40s. But getting older doesn’t necessarily mean you’ll get gum disease. Daily dental care and regular visits to your dentist can reduce your risk of gum disease.
Smoking greatly increases your risk for periodontitis—another reason not to smoke. Other factors that boost your risk include hormonal changes in women, certain medications and some illnesses like diabetes, cancer and AIDS.
NIH-supported researchers are working to learn more about preventing and treating gum problems. Some are exploring whether stem cells might help to restore damaged tissues that support the teeth. Others are searching for genes and proteins produced by our bodies and by the bacteria in our mouths to see how they interact to affect gum health.
Some studies suggest that gum disease may increase the risk of heart attack or stroke or cause other health problems. But so far, it hasn’t been confirmed that gum disease contributes to these conditions. Although many aspects of gum disease are still being investigated, one thing is clear: controlling gum disease can save your teeth. That alone is an excellent reason to take good care of your teeth and gums every day.
Keep Your Mouth Healthy
Oral Care for Older Adults

Oral health is important for people of all ages. But the simple routine you learned as a kid—brush your teeth twice a day and floss regularly—can become more of a challenge as you get older. Among adults ages 75 and up, about 1 in 4 has lost all natural teeth, largely because of gum disease and tooth decay.
You can take steps to keep your mouth healthy throughout your lifetime. And if you’re a caregiver for an older adult, you can help ensure that he or she gets proper oral care. Tooth decay and gum disease don’t have to be a part of getting older.
“We have to worry about the same conditions throughout life, although some conditions are more prevalent at certain ages,” says Dr. Dena Fischer, a dental health expert at NIH. The 2 most common oral health problems are tooth decay (cavities) and gum disease. “Gum disease is more common when you’re older,” Fischer explains. “But cavities can happen at any age, as long as you have natural teeth.” Both are largely preventable with proper care.
Cavities develop as plaque builds up on your teeth and under chipped fillings, producing acids that can eventually eat away at the tooth’s hard outer surface.
Gum disease is an infection of the gums and surrounding tissues that hold your teeth in place. Gum problems arise as plaque builds up along and under your gum line. In severe cases, the bone and tissue that hold teeth in place can break down, and teeth may eventually become loose and have to be removed.
Reduce your risk of developing tooth decay and gum disease by brushing daily with fluoride toothpaste and flossing. Also visit the dentist regularly for a cleaning and checkup.
Another common problem for older adults is dry mouth. Dry mouth occurs when you don’t have enough saliva, or spit, to keep your mouth wet. “Saliva is very important,” Fischer says. “The protective factors in saliva prevent cavities, gum disease, and fungal infections.”
Dry mouth can be caused by medications; alcohol or tobacco; or medical conditions, such as poorly controlled diabetes. Dry mouth is usually treatable, so talk with your doctor or dentist if you’re having problems.
Older adults are also at increased risk for oral cancer. Symptoms include a sore, irritation, or lump in the mouth or throat that lasts more than two weeks; it may be painful or may cause numbness. It’s important to catch oral cancer early, because treatment works best before the disease has spread. Be on the lookout for any changes in your mouth, especially if you smoke or drink.
If you serve as a caregiver to an older adult, you can help that person overcome oral health challenges. Encourage him or her to use an electric or large-handled toothbrush, so it’s easier to grip. You might place your hand over his/hers to help guide the toothbrush. Dentures should soak in water overnight and once a week with a denture cleaner. Dentures should also be rinsed after each meal and brushed daily.
A healthy mouth can help you eat well, avoid pain, and feel good about yourself. Take steps to keep your mouth healthy, whatever your age.
Diarrhoea
Prevention Diarrhoea is often caused by an infection. You can reduce your risk by making sure you maintain high standards of hygiene. For example, you should: • wash your hands thoroughly with soap and warm water after going to the toilet and before eating or preparing food • clean the toilet, including the handle and the seat, with disinfectant after each bout of diarrhoea • avoid sharing towels, flannels, cutlery or utensils with other household members It’s also important to practise good food and water hygiene while travelling abroad, Avoid dehydration; drink clear fluids, preferably those containing electrolytes and an energy source such as glucose. Simple Gatorade is an option but rehydration sachets or solutions can be bought over the counter from a pharmacist or obtained on prescription from your doctor.
Fight Off Food Poisoning
Food Safety for Warmer Weather

In warm-weather months, who doesn’t love to get outside for picnics, backyard gatherings, and of course delicious foods? But high temperatures raise your chance of getting sick from things you eat. Learn how to handle food properly to avoid the misery of food poisoning.
It can be hard to keep foods safe to eat during warmer weather. If you’re eating or preparing foods outside, you may have trouble finding places to wash your hands, keep foods cold, or cook at the proper temperature—all of which are important to prevent foodborne illness.
“Food poisoning occurs if the foods you eat contain certain microbes or the toxins they produce,” says Dr. Alison O’Brien, a food safety expert at the Uniformed Services University of the Health Sciences in Maryland. “You can get sick directly from swallowing the toxins. Or you can get sick if the microbes get into your gut and start to multiply.”
Each year, about 1 in 6 Americans get sick from tainted foods. Most foodborne illnesses arise suddenly and last only a short time. But food poisoning sometimes leads to more serious problems. Foodborne diseases kill about 3,000 people nationwide each year. Infants, older people, and those with compromised immune systems are especially at risk.
Many people know the symptoms of food poisoning: vomiting, diarrhea, abdominal pain, fever, or chills. The sickness may be mild or severe. It may last from a few hours to several days. The symptoms and length of illness depend on the type of disease-causing microbe or toxin you’ve swallowed.
The leading cause of foodborne disease outbreaks in the U.S. is norovirus. This highly contagious virus sickens more than 20 million people nationwide each year, leading to vomiting and diarrhea. Norovirus outbreaks can occur anywhere people gather or food is served.
“You can get norovirus when a sick food handler contaminates your food, possibly by not washing their hands well enough after touching the virus,” O’Brien says. “Swallowing just a little norovirus can make you very sick.”
Several types of bacteria can also cause food poisoning. Some foods you buy—such as raw meat or fruits and vegetables—may already contain bacteria that you need to wash off or cook to destroy. Bacteria can also thrive in certain foods if not stored properly.
Bacteria like Staph and Bacillus cereus can make you sick quickly, within 1 to 7 hours. These bacteria produce fast-acting toxins in foods (such as meat or dairy for Staph, and starchy foods like rice for B. cereus). Keeping such foods refrigerated at 40 °F or colder helps slow or stop the growth of these bacteria.
Other bacteria, such as Salmonella and Campylobacter, don’t make you sick until they get in your body and multiply. With these microbes, it can take 12 hours or a few days for you to feel ill. “Symptoms can include fever, cramps, and sometimes bloody diarrhea,” says O’Brien.
When you have a foodborne illness, you usually need to drink plenty of fluids. “But see a doctor if you have blood in your stool,” O’Brien advises. “And if a child seems to have food poisoning, you should have the child seen by a doctor.”
Good hygiene, particularly washing your hands thoroughly after going to the toilet, is essential in case the diarrhea is infectious.
- Do not prepare food for other people, especially babies and old people, while you have acute diarrhea.
- A carbohydrate diet that includes boiled potatoes or boiled rice may help.
- If the diarrhea does not resolve after a few days, seek medical advice.
- Stop eating and drinking for a few hours. Try sucking on ice chips or taking small sips of water. You might also try drinking clear soda, clear broth or noncaffeinated sports drinks. You might also try oral rehydration solutions if you have severe dehydration symptoms or diarrhea Prevención La diarrea a menudo es causada por una infección. Puede reducir su riesgo asegurándose de mantener altos estándares de higiene. Por ejemplo, debe: • lavarse bien las manos con jabón y agua tibia después de ir al baño y antes de comer o preparar alimentos • limpiar el baño, incluido el asa y el asiento, con desinfectante después de cada episodio de diarrea • evitar compartir toallas , franelas, cubiertos o utensilios con otros miembros del hogar También es importante practicar una buena higiene de los alimentos y el agua al viajar al extranjero, Evitar la deshidratación; beba líquidos claros, preferiblemente aquellos que contienen electrolitos y una fuente de energía como la glucosa. Gatorade simple
Pink Eye Conjunctivitis
- Pink eye is redness and swelling of the eye surface and the conjunctiva
- Wash your hands often. Always wash them before and after you treat pink eye or touch your eyes or face.
- Use moist cotton or a clean, wet cloth to remove crust. Wipe from the inside corner of the eye to the outside. Use a clean part of the cloth for each wipe.
- Put cold or warm wet cloths on your eye a few times a day if the eye hurts.
- Do not wear contact lenses or eye makeup until the pink eye is gone.
- If the doctor gave you antibiotic ointment or eyedrops, use them as directed. Use the medicine for as long as instructed, even if your eye starts looking better soon. Keep the bottle tip clean, and do not let it touch the eye area.
- To put in eyedrops or ointment:
- Tilt your head back, and pull your lower eyelid down with one finger.
- Drop or squirt the medicine inside the lower lid.
- Close your eye for 30 to 60 seconds to let the drops or ointment move around.
- Do not touch the ointment or dropper tip to your eyelashes or any other surface.
Pink Eye
- Have you ever looked in the mirror and found the whites of your eye have turned pink? That’s a main symptom of conjunctivitis, more commonly known as pink eye.
- Pink eye is an inflammation of the outer layer of the eye and inside the eyelid. Your eyes turn red and irritated, and have a weepy discharge. It’s often caused by viruses, bacteria or allergies.
- “Conjunctivitis can be contagious, and typically spreads from person to person through hand contact with someone who is infected,” says Dr. Nida Sen, an NIH ophthalmologist and researcher. “Use separate towels, disinfect toys and other objects that are frequently handled, and make sure everyone who might be exposed washes their hands often.”
- Treatment for pink eye depends on its cause, which can be determined by an eye care professional. If it’s bacterial, your doctor may prescribe antibiotic drops or ointment. If it’s viral, the infection will likely clear up on its own. If allergies are the cause, eye drops for allergies might help.
- “In most people, pink eye causes no lasting problems, but in rare cases it can be associated with a more serious disorder,” Sen says. “If you notice a change in your vision, you should inform your eye care professional.”
- Do not share towels, pillows, or face cloths while you have pink eye.
Lávese las manos a menudo. Siempre lávelos antes y después de tratar el conjuntivitis o tocarse los ojos o la cara. Use algodón húmedo o un paño limpio y húmedo para eliminar la corteza. Limpie desde la esquina interior del ojo hacia el exterior. Use una parte limpia del paño para cada toallita. Ponga paños húmedos fríos o tibios en el ojo varias veces al día si le duele el ojo. No use lentes de contacto ni maquillaje para los ojos hasta que desaparezca el ojo rosado. Si el médico le administró ungüento antibiótico o gotas para los ojos, úselos según las indicaciones. Use el medicamento durante el tiempo indicado, incluso si su ojo comienza a verse mejor pronto. Mantenga la punta de la botella limpia y no deje que toque el área de los ojos. Para poner en gotas o ungüento para los ojos: Incline la cabeza hacia atrás y baje el párpado inferior con un dedo. Deje caer o rocíe el medicamento dentro del párpado inferior. Cierre el ojo durante 30 a 60 segundos para que las gotas o el ungüento se muevan. No toque la pomada o el gotero de la punta de sus pestañas o cualquier otra superficie. No comparta toallas, almohadas o toallitas faciales mientras tenga ojo rosado.
Protect From Lyme Disease

The most common disease ticks carry is called Lyme disease. It’s a bacterial infection that can cause serious health problems.
Each year, an estimated 300,000 people in the U.S. get Lyme disease. The number of cases has risen dramatically over the last 10 years. Symptoms of Lyme disease can include fever, headache, muscle or joint pain, and extreme fatigue.
People with Lyme disease usually get an expanding red rash that can resemble a bull’s-eye. If left untreated, the infection can spread and cause rashes in other parts of the body. Some people may develop nerve pain, arthritis, or heart problems. Most people fully recover when treated with antibiotics, especially when Lyme disease is diagnosed early.
The deer ticks that carry Lyme disease can be as small as a poppy seed. You might not even know you’ve been bitten. Preventing tick bites is the best defense against Lyme disease. You can protect yourself and your family by using insect repellent when going places where ticks are likely to live.
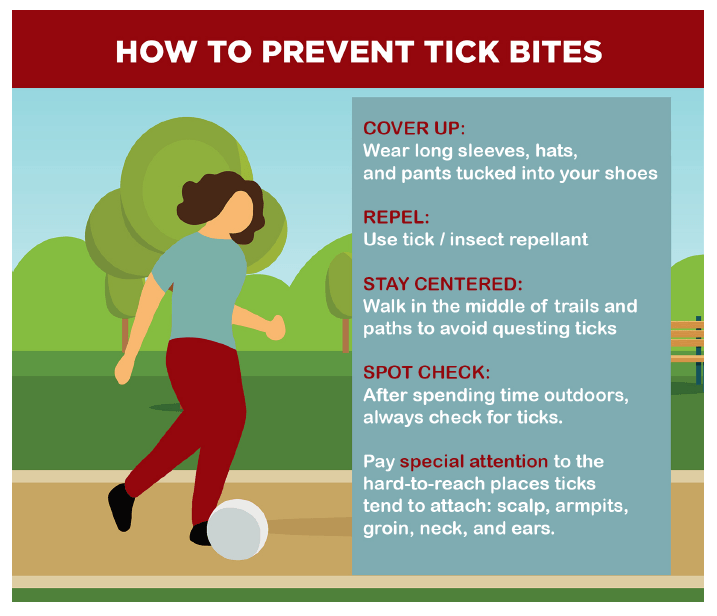
After coming indoors, check your clothing and gear for ticks. Shower within two hours of coming indoors. Then conduct a full body check. Don’t forget to check your hair, where ticks may be harder to spot.
Oral antibiotics are the standard treatment for early-stage Lyme disease. Most people who develop Lyme disease recover fully following a course of antibiotics. You should consult your Doctor or a specialist for diagnosis and treatment of Lyme Disease.
Citation: NIH
Get the good fats — the good, the bad
Good fats are essential to your diet. They help you absorb vitamins, speed up your metabolism, and help regulate your blood sugar. They can also lower your risk for obesity and diabetes, high blood pressure and heart disease,
Bad fats can make you unhealthy and can contribute to inflammation and heart disease. Use these tips to get your fat intake

Reduce the amount of trans fat you eat
- Eat more vegetables, fruit, and unprocessed whole grains: these foods contain no trans fat.
- Avoid deep fried foods. ...
- Cook at home whenever you can. ...
- Bake and cook with a soft, non-hydrogenated margarine instead of hard (stick) margarine, butter or shortening.
The American Heart Association recommends about 13 grams of saturated fats per day.
That means significantly reducing daily red meat and excessive dairy Saturated fats are naturally found in animal fats, dairy and foods like these:
- Red meat – beef, pork, lamb, veal, poultry skin.
- Whole milk.
- High-fat cheese.
- Butter.
- Ice cream.
- Tropical oils – like palm and coconut.
Get good fats on your grocery list Start by shopping for whole or unprocessed plant foods like:
- Avocados.
- Coconuts.
- Nuts — including nut butters and oils.
- Seeds — including seed butters and oils.
- Poultry.
- Fish.
Eat foods with monounsaturated fats
Monounsaturated fats are healthy fats that can help reduce bad cholesterol levels in your blood — which can lower your risk of heart disease and stroke. They provide nutrients to your cells and vitamin E, a beneficial antioxidant.

include plant-based liquid oils such as:
- olive oil,
- canola oil,
- peanut oil,
- safflower oil and.
- sesame oil.
Stock up on plenty of polyunsaturated fats
“Polyunsaturated fats are healthy fats that provide the same benefits as monounsaturated fats, but also include omega-3 and omega-6 fatty acids – fats that your body can’t produce itself. So to get them, you must add foods that contain them into your diet,” Lachman says. Cook with and/or use plant-based liquid oils in your recipes like:
- Soybean oil.
- Corn oil.
- Sunflower oil.
- Walnut oil.
- Olive oil.
Shop for these seeds and beans, too:
- Walnuts.
- Sunflower seeds.
- Tofu.
- Soybeans.
- Flaxseed.
- Pumpkin seeds.
Eat plenty of oily, cold-water fish like:
- Salmon.
- Tuna.
- Sardines.
- Mackerel.
- Trout.
- Herring.
Add these whole grains to your grocery list (they’ll also help keep you lean):
- Brown rice.
- Wheat.
- Oatmeal.
Eat diet with these daily meal tips
Breakfast boost — Instead of high-fat cream cheese and a bagel at breakfast, cook a batch of oatmeal and sneak in some flaxseed to give your body a little extra omega-3 bright and early. Replace your high-fat coffee creamer with a little real cream, milk (or non-dairy variety) or see if you can learn to savor your cup of joe black.
Lighten your lunch — Add avocado to sandwiches and salads instead of using condiments or dressings to lower your saturated fat intake. Add skinless chicken to your favorite salads instead of bacon. Skip the high-fat cottage cheese and swap it out for the reduced-fat kind. A fat-friendly dinner — For dinner, crush up nuts and sprinkle them over a piece of salmon or your favorite oily fish before cooking. Use canola or olive oil instead of butter to sauté it – as well as your favorite vegetables. Skip cream-based sauces and choose vegetable or nut butter sauces instead.
Snack smarter — Eat olives (not the ones stuffed with cheese) for your mid-day or late-night snack instead of potato chips or pretzels. You’ll still get a bite-sized treat, but with high amounts of monounsaturated fat and fewer calories.
Whip up some spreads that are ready for anytime — Grind nuts in a food processor and store to use later as all-natural nut butter on your toast or rice cakes in the morning, or for a healthy snack during the day. You’ll get the bonus of a powerful protein-packed snack, too.
“The benefits of good fats are vast. Enjoy, control your portions, and you’ll begin to see changes in how you’re feeling overall.”
Common Skin Conditions
What do your bumps, blisters, and rashes mean?
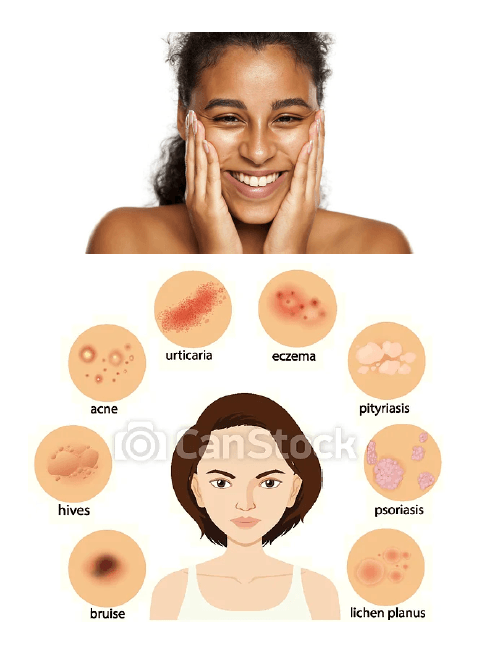
If you have skin problems that keep coming back, you may need to speak to a dermatologist.
Skin: It's our body's largest organ. It protects us by keeping fluids in and harmful microbes out.
Sometimes, due to our environments and genes, our skin gets, well, unhappy. But how can you tell the difference between a minor rash and a more serious condition? Read our quick rundown of five common skin conditions and what they look like. Also, be sure to talk to a dermatologist, a doctor who specializes in skin conditions, or other health care provider for a full diagnosis and care.

Hives
Hives are pink, itchy bumps that can appear anywhere on the skin and last for less than 24 hours. They may be caused by some food allergy, infection, or medications. Hives are common and often go away on their own.

Eczema
Eczema, or atopic dermatitis, often begins before age 5 and may continue as kids get older. For some people, the raw, sensitive, and inflamed skin may cause severe itching at night. It often happens on the face, inside the elbows, behind the knees, and on the hands and feet.

Contact dermatitis
Contact dermatitis may have well-defined borders and appears when your skin touches a foreign substance (dyes, soaps, latex, poisonous plants). The resulting rash may be itchy and red, and oozing blisters may develop. The reaction most often occurs 24 to 48 hours after the exposure.

Psoriasis
Psoriasis consists of thick patches of rough, scaly skin, most commonly on the scalp, elbows, knees, and lower back. These patches can be itchy and painful and may bleed when scratched. Psoriasis sometimes runs in families and can be associated with arthritis that often involves the fingers, toes, or spine.

Dry skin
Dry skin occurs when your skin loses too much water and oil. It can happen at any age. The rough, cracked, and itchy skin may be caused by cold, dry air; washing your hands often; harsh soaps or detergents; and aging. As we get older, our skin makes less natural oil.
Source: National Institute of Arthritis and Musculoskeletal and Skin Diseases